
views
Recognizing Symptoms
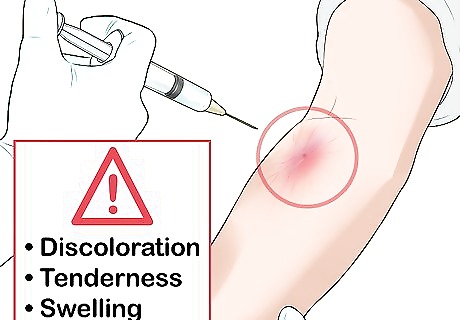
Look for changes around the injection site. Common symptoms of a collapsed vein are discoloration, tenderness, and swelling. Monitor the area where the needle was inserted for atypical bruising, discoloration, or sensitivity to touch. A large collapsed vein may also cause extremities such as hands or feet to feel cold, but this is typically more a symptom of a collapsed artery, which is a different and more critical issue.

Inspect the injection site. If your vein has collapsed, you’ll experience sharp pain at the injection site. The site may also bruise, or appear black and blue. The injection site may also become itchy.

Avoid scratching at the injection site. If the injection site begins to itch, this is actually a good sign. While it confirms that the vein was collapsed, the itching indicates that blood is starting to reopen the vein and recirculate. Scratching the itch, however, can interrupt this process and risks permanently damaging the vein.
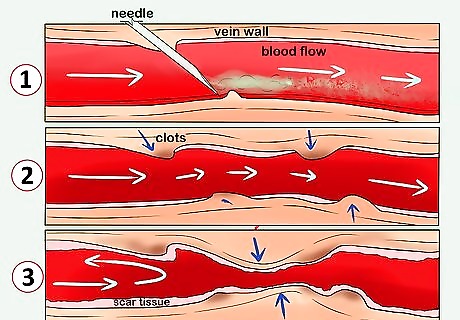
Understand long term effects. Nearly every intravenous drug user will experience a collapsed vein at some point during their drug use. Often, veins will reopen on their own. When they do not, serious, permanent health complications can follow, including inadequate circulation. Ultimately, very little can be done about a collapsed vein. As such, it is vital to focus on preventing your veins from collapsing.
Seeking Treatment
Recognize the severity of a collapsed vein. Many collapsed veins cannot heal. Permanent damage can also occur in a very short amount of time. If you believe you have a collapsed vein, contact a doctor or clinic to discuss treatment options. In order to give a vein its best chance to heal, stop injecting into that vein altogether.
Ask a medical professional about supplements that may help. Vitamin C and other supplements may help fight inflammation within the veins. That said, no supplement will eliminate the risk of a collapsed vein, nor guarantee that a collapsed vein will fully heal. It’s always best to see a medical professional immediately if you believe you may have a collapsed vein.

Anticipate medication or surgery. If you are diagnosed with a recently collapsed vein, a doctor may prescribe blood thinners that will help thin your blood and encourage it to circulate. In other cases, they may recommend surgery to repair damaged veins as much as possible.
Avoiding Collapsed Veins

Get help quitting intravenous drug use. The best way to avoid a collapsed vein is to eliminate the behavior that causes them. It can be hard to quit using drugs, especially if you’ve been using for a while. Fortunately, there are resources available to help you quit. Start by taking the first step and asking for help.
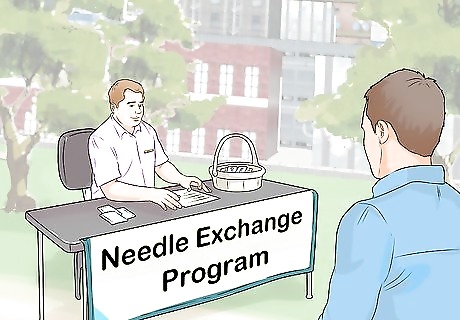
Exchange your needles. If you have decided not to quit, there are steps you can take to make intravenous drug use less dangerous. Foremost, find a needle exchange program in your area and use it. Used needles with blunted ends are one of the most common causes of collapsed veins.
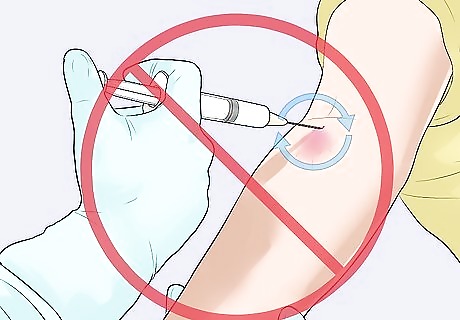
Do not repeatedly use the same injection site. Collapsed veins are often the result of repeated vein trauma in the same area. Avoid regularly injecting in the same site. Never inject into a site that is visibly swollen or bruised.
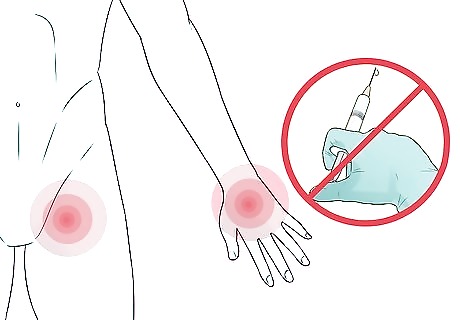
Avoid injecting into your hand or groin. Veins in your hands are small, and will collapse easily. Similarly, injecting into veins in your groin can cause especially dangerous circulation problems.
Clean the area and the needle before injecting. Dirt and other debris can enter your vein and cause irritation that may lead to collapse. Accordingly, wipe down the area you will inject as well as the needle before use.
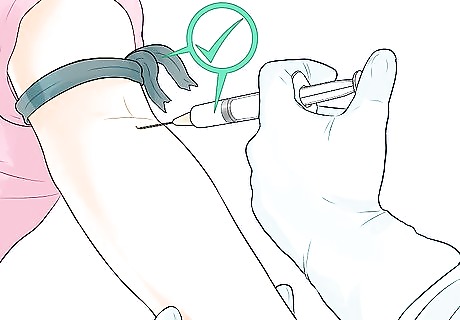
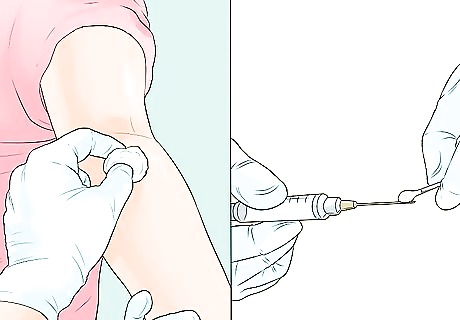
Perform injections slowly and carefully. There are many aspects of non-medical intravenous injections that can be dangerous. For instance, a tourniquet should never be tied too tightly, and a needle must be removed slowly after injecting.
















Comments
0 comment