
views
X
Research source
For those who have had their lymph nodes removed or negatively impacted by radiotherapy, you may experience swelling in your face called lymphoedema. There are specific methods you can use to help reduce swelling due to lymphoedema.[2]
X
Trustworthy Source
National Health Service (UK)
Public healthcare system of the UK
Go to source
At-Home Therapies

Keep your head elevated above your heart. Once you’re home from surgery, keep your head elevated at all times, even when you’re sleeping. Use 2-3 pillows in your bed to prop yourself up, or even try to sleep in a reclining chair. If you opt to lie on the couch, use the arms of the couch or couch cushions to prop yourself up. Swelling is caused by the excess build-up of blood and fluids in and around the area where the surgery took place. Keeping your head elevated will help those fluids flow away from the surgical area and should help prevent or reduce the amount of swelling you experience.
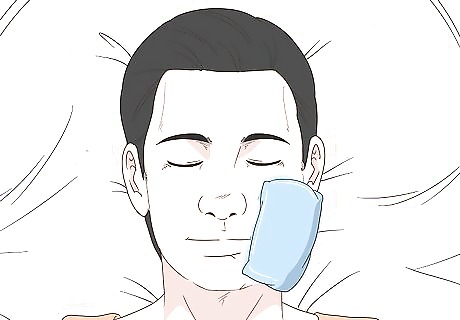
Use ice to reduce swelling immediately following surgery. During the first 48 hours after surgery, use an ice or cold pack on the areas of your face that are swollen. Keep the ice or cold pack on for 20-30 minutes at a time and then remove it for 20-30 minutes before applying it again. Place a towel or cloth between the ice/cold pack and your face so you don’t damage your skin. Instead of ice or cold packs, you can also use a bag of frozen vegetables or crushed ice inside a resealable plastic bag. Use a cloth or towel between the bag of veggies and your skin.
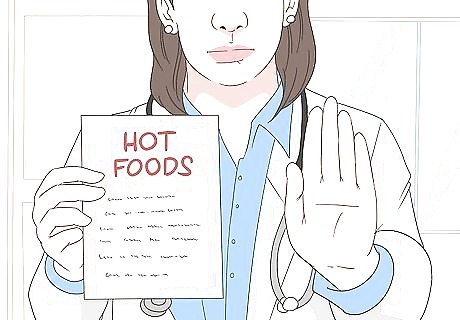
Do not eat or drink hot items if you’ve had oral surgery. For the first 24-48 hours after oral surgery, avoid eating or drinking anything hot (e.g., coffee, hot chocolate, soup, etc.). The heat in the food and drinks may actually increase the amount of swelling you experience inside your mouth. Your doctor may also give you a list of other foods to avoid for a certain period of time as your mouth heals. Some foods may be too harmful to your incisions to eat right away. Your doctor may also ask you to avoid hot foods/drinks for shorter or longer than what is mentioned here, depending on the extent of the surgery you’ve had.
Stick to drinking from a cup, not through a straw. If you’ve had oral surgery, especially a tooth extraction, avoid drinking any kind of liquid through a straw for at least 48 hours. Doing so could dislodge the blood clot that forms in the empty socket, leading to intense pain and possibly an infection or more inflammation. While this sounds pretty scary, try not to worry. If you do get dry socket, your dentist or oral surgeon will be able to treat the problem and provide quick pain relief. With proper treatment, this condition doesn’t usually cause any serious complications.

Avoid smoking and drinking in order to heal quickly. If possible, stop smoking 8 weeks in advance of surgery to reduce complications. At the very least, stop smoking and drinking alcohol after your surgery and do not restart until you’re healed. Tobacco and alcohol can actually slow down your body’s ability to heal and can increase your risk for infections. Smoking reduces the amount of oxygen in your blood, which can make it hard to prevent or heal from an infection. Alcohol reduces the effectiveness of your heart and immune system, which can cause complications after surgery.

Rinse your mouth with saltwater starting 24 hours after oral surgery. Immediately following oral surgery, avoid rinsing out your mouth with any type of liquid. For the first 24 hours, you want your blood to clot in and around the incisions in your mouth. Rinsing your mouth during this time may dislodge the blood clots and cause bleeding. Once 24 hours have passed, rinse your mouth with saltwater 4 times a day. Mix 1 tsp (4.9 mL) of salt with a glass of warm tap water to create a saltwater rinse. Do not swallow the saltwater. Always spit it back out into the sink. Rinse your mouth 4 times a day for at least 4-5 days or until you can start brushing your teeth again.

Use nose sprays to keep your nasal passages open if needed. If you’ve had any type of surgery on or around your nose or nasal passages, you’ll need to use nose sprays to keep those passages open so you can breathe properly. Use an over-the-counter saline spray (whichever one is recommended by your doctor) every 2-3 hours to keep your nasal passages open and comfortable. You may also find it helpful to have a humidifier in your bedroom while you’re healing, which will also help keep your nasal passages moist and clean. As much as possible, avoid blowing your nose if you’ve had surgery on your nose or throat. The pressure could cause your incision(s) to open up again. Your surgeon will tell you when you can safely blow your nose again.
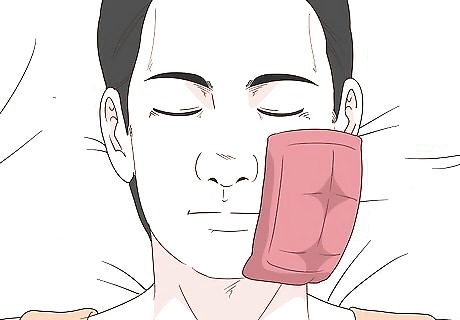
Use a warm compress after 48 hours have passed. Once the first 48 to 72 hours have passed since your surgery, or once you notice the swelling has started to decrease, you can change from ice and cold packs to warm compresses. Use a warm compress or heating pad (on a low setting) on the swollen area of your head or face 4 times per day for 30 minutes at a time. The warmth will increase the blood flow to the area, which will help reduce swelling and speed up the healing process.
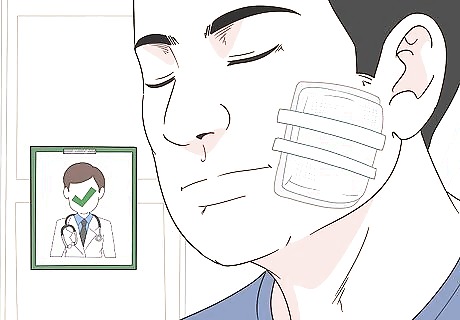
Change your bandages and clean your incision as directed. If your surgery results in an incision on your face, you may have stitches and/or bandages over that area. Follow your doctor’s instructions as to how often to change the bandages and how to clean the wound. Keep the area dry as per your doctor’s instructions and be on the lookout for any possible infections. Incisions will normally be sore, tender, or numb. They may also feel tingly or itchy. Signs of infection include green or yellow discharge, redness or hardening around the incision, skin around the incision being hot to the touch, fever, increased or unusual pain, and excessive bleeding.
Get up and walk around to heal faster. While you’ll likely be tired and uncomfortable immediately after surgery, start to move around after 24-48 hours of bed rest. Moving around your home will help get the blood flowing through your body, which in turn will help speed up the healing process and reduce swelling. Sitting or lying still for too long, even propped up, may actually cause you to take longer to heal. Follow your doctor’s instructions regarding movement and exercise after surgery.
Treating Lymphoedema

Take extra care of the skin on your face to prevent infection and injury. When you have lymphoedema, any injury or infection that impacts the skin on your face can make the swelling worse. This means you need to avoid getting sunburns, insect bites, scratches, bruises, and cuts on your face or inside your mouth. If you do experience an injury, cut, or scratch to your face, wash the area immediately and apply an antibiotic ointment. If you notice an infection starting, see your doctor right away. Only use soap-free cleansers to wash your face. Use an electric razor to shave, rather than a manual one. Moisturize your face and neck every day with an unscented cream or lotion. Protect your face from the sun by wearing a hat and using (at least) 30 SPF sunscreen. Use insect repellent to prevent stings and bites from irritating your skin. Signs of infection include green or yellow discharge, redness or hardening around the incision, skin around the incision being hot to the touch, fever, increased or unusual pain, and excessive bleeding.
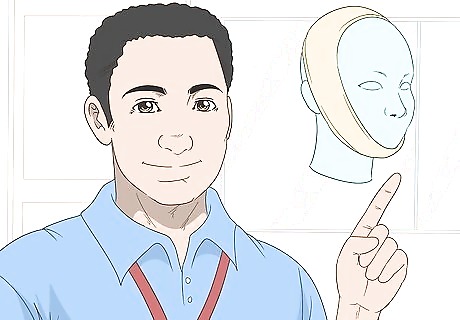
Ask your physical therapist about compression garments. Compression garments work best if they’re used immediately following cancer treatment. Therefore, before cancer surgery, speak to your physical therapist about any compression garments they’d recommend you use for your specific situation. Wash your compression garment every 1-2 days by hand to keep it clean. Do not use a compression garment if it causes pain or discomfort. Compression garments used to reduce facial swelling include full face masks and straps that wrap around your chin and the top of your head. Some surgeons apply tight compression wraps that you’ll wear long-term in between treatments to prevent lymph from pooling in your tissues. They may re-apply the wrap at each treatment.

Try to sleep with your head propped up to prevent swelling overnight. Unfortunately, gravity will play a role in the swelling you experience. This means your lymphoedema may be at its worst first thing in the morning, after you’ve been lying down for many hours. To help prevent excess swelling first thing in the morning, sleep with your head propped up on a couple of pillows. Some of this excess overnight swelling will disappear once you get up and start moving around.

Wear baggy clothing and forego jewelry on your neck or face. Anything that can cause constriction around the area which is swollen can not only cause damage, but can impact your ability to breathe and function. Wear clothes that are baggy around your neck. Do not wear necklaces. Be careful of any facial piercings you may have—you may want to remove them and leave them out. If you experience lymphoedema in more than just your face and neck, wear clothing that’s baggy around those areas as well. If you experience lymphoedema in your arms, do not wear bracelets or watches.
Taking Medications as Directed
Continue your prescription antibiotics until they’re done. Your doctor has likely prescribed antibiotics to take after surgery to prevent infection. Take the full prescription as directed; do not stop early even if you feel better or you don’t have any signs of an infection. Infections, unfortunately, will cause even more swelling in the area and will slow down the healing process. Most infections will show up within 30 days of surgery. They’ll cause the area to be red, painful, and even hot to the touch.

Use nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce swelling. Take an over-the-counter NSAID pain reliever as recommended by your doctor to help reduce swelling and pain. If your doctor doesn’t recommend a specific brand, ask your pharmacist for advice. Take the NSAID pain reliever as instructed by your doctor, by your pharmacist, or via the instructions on the label. NSAID pain relievers can be found at any drug store or pharmacy, as well as online. If your doctor provides you with a prescription pain reliever, take that prescription pain reliever instead of the NSAID pain reliever (unless otherwise directed). Speak to your pharmacist about interactions between any prescription drugs you’re currently taking and NSAID pain relievers.

Take corticosteroids if given a prescription. Corticosteroids include both natural and synthetic hormones that are specifically designed to reduce inflammation. Your doctor may prescribe them if they feel the swelling needs some additional help to decrease. Corticosteroids may be prescribed in pill form, as a nasal spray, as eye drops, or as a cream. Follow the instructions provided by your doctor or pharmacist for the corticosteroid you’ve been prescribed. Unfortunately, corticosteroids can sometimes make swelling worse. If your facial swelling increases or doesn’t improve after you start steroids, talk to your doctor or surgeon about whether this might be a side effect of the steroids.
















Comments
0 comment