views
Assessing Someone Who Is Choking
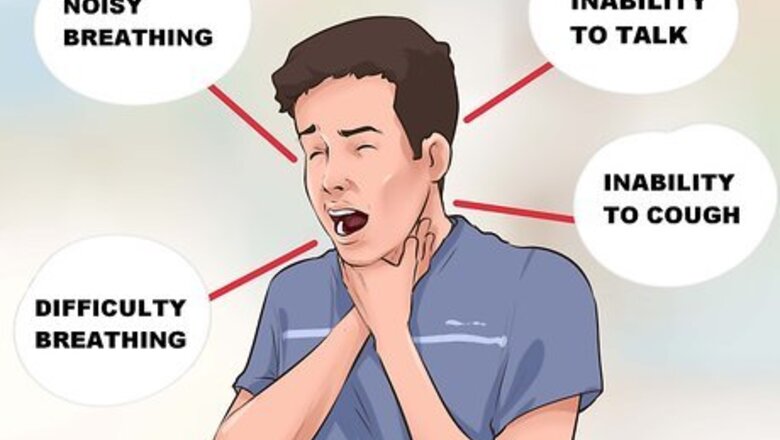
Look for classic signs of choking. Someone who is choking may display the following symptoms: Difficulty breathing Noisy breathing Inability to talk Inability to cough Skin turning blue (called "cyanosis," which is due to lack of oxygen circulating in the blood) Decreasing level of consciousness

Tell someone to call emergency services. It is important to call emergency medical personnel via 911 or a local number immediately when a person is choking; more than three to five minutes without oxygen to the brain will likely result in death.

Understand the Red Cross recommendations for a person who is choking. These include alternating between five "back blows" and five "abdominal thrusts" (also known as the Heimlich maneuver), repeating the cycle until the object is dislodged, emergency personnel arrive, or the victim becomes unconscious due to lack of oxygen. Back blows are a forceful motion with the heel of your hand between the person's shoulder blades, when he is bending over so that his trunk is at least parallel to the ground (this way, if you successfully dislodge the obstructing object it will fall with gravity out of the victim's airway). The back blows are optional, depending on whether you have been trained how to effectively do these (if not, skip them and do only "abdominal thrusts," which are described in the next section).
Performing Abdominal Thrusts

Reach around the victim from behind. Circle your hands around the victim's abdomen (stomach). If the victim is sitting or standing, position yourself directly behind her. If the victim is lying down, lay behind her. If the victim is already unconscious, check for a pulse. If there is no pulse, proceed straight to CPR (cardiopulmonary resuscitation) at a rate of 100 chest compressions per minute. Do not attempt abdominal thrusts at this time (and do not do rescue breaths in this situation as the airway is obstructed).
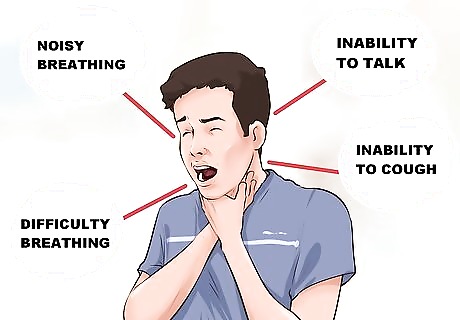
Make a fist with your dominant hand. Your thumb should point into the fist. Place this fist just above the victim's navel (belly button) and under the breastbone.

Wrap your other hand firmly around this fist. Be sure to keep your thumb away from the victim's body to prevent injury to the victim.

Pull inward and upward, pressing into the victim's abdomen with quick, forceful upward thrusts. Make the motion similar to the letter "J" – in, then up.

Continue to perform the Heimlich maneuver. Do this as long as the person maintains some breathing sounds (including gasping, choking, or any audible air motion). If the person is unable to breathe at all, and the Heimlich maneuver is unsuccessful at dislodging the object, proceed to tracheotomy. This is a risky procedure and should only be used as a last resort; if possible, it should be performed by a medical professional.
Performing the Tracheotomy

Call 911 before you begin. Make sure that you call 911 before you begin to make sure that performing a tracheotomy is even necessary. The emergency response team may be nearby. If you truly have no other option but to perform a tracheotomy, then you should still stay on the phone with emergency services. The dispatcher may be able to talk you through the procedure or put you in contact with someone who can. Having someone on the phone may also help to keep you calm.
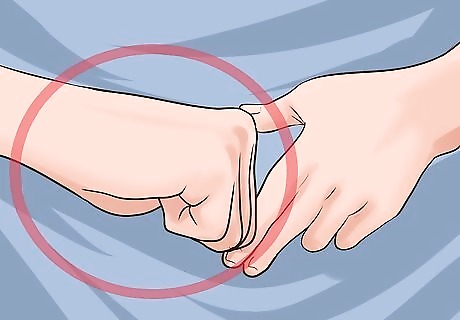
Find the area over the cricothyroid membrane on the victim’s neck. This is the soft spot on the throat where the incision will be made. To find this, find the Adam's apple, or larynx. Both men and women have an Adam's apple, but they are more pronounced on adult men. You may have to feel the victim's neck to find the Adam's apple on a woman or a child. Slide your finger down from the Adam's Apple until you feel another bulge; this is the cricoid cartilage. There is a slight indentation in between the Adam's Apple and the cricoid cartilage; this is where the incision will be made.
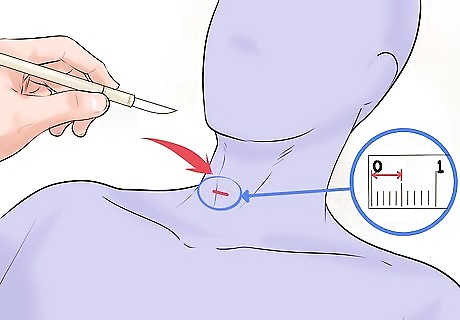
Make a half-inch horizontal cut about a half-inch deep. Just below your cut, you'll see the cricothyroid membrane (it is a yellowish elastic membrane located between the surrounding layers of cartilage). Make an incision on the membrane itself. The depth of the puncture should be just sufficient to gain access to the airway. Given the emergency nature of this procedure, it is okay to proceed without formal sterilization. Time is of the essence, and the concern of potential infection can be dealt with when emergency medical personnel arrive. However, if gloves are available — even if they are not sterile — use them to protect yourself from bloodborne diseases like HIV and hepatitis.
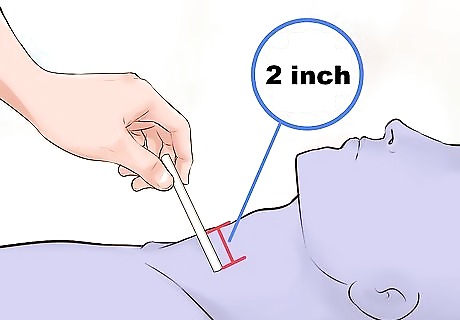
Maintain the opening to facilitate breathing. Do this by placing a straw tube 2 inches (5.1 cm) into the trachea. You can suck on the straw and see if you get air coming back to you to confirm that it is correctly located in the victim's airway. A ballpoint pen casing (with the ink-filled tube from the inside removed) is also a good option for a tube.

Administer two breaths through the breathing tube. These should last approximately one second each. Hopefully, the victim will begin breathing on her own (you will see her chest rise and fall if she is breathing on her own). If the victim is breathing on her own, continue to supervise her and wait for emergency medical personnel to arrive to deal with the situation more definitively. If the victim is not breathing on her own, continue giving breaths and check for a pulse. In the absence of a pulse, proceed to CPR. The cycle for CPR is 30 chest compressions (at a rate of approximately 100 chest compressions per minute) followed by two rescue breaths through the breathing tube. Repeat this cycle approximately five times. If the victim is unresponsive after five cycles, use an AED (automated external defibrillator) if you have been trained how to do so. If not, follow instructions from emergency medical personnel who can give directions over the phone while you await their arrival. Note that if you are untrained in CPR, the chest compressions are more important than the rescue breaths, so it is okay to do chest compressions only (at a rate of 100/minute) and to omit the breaths until emergency medical personnel arrive. Remember that doing something is better than nothing, as someone's life is on the line here!












Comments
0 comment