
views
X
Research source
Pearson M. Guideline for Prevention of Intravascular Device-Related Infections. The Hospital Infection Control Practices Advisory Committee, Centers for Disease Control and Prevention, Atlanta, USA. 199
Only change an IV if you are a nurse or an authorized medical worker.
Preparing to Change the IV
Check the doctor’s order sheet and the IV sheet for the patient. Counter check the IV label, the bottle number, the type of solution, the amount of solution, the additives(if necessary), the duration of infusion and the IV flow rate. Confirming all of these details will ensure the patient receives the right amount and type of IV solution. Always counter check the data in the patient’s chart because the doctor’s orders vary from person to person, For example, patient 1 and 2 may have the same type of IV fluid but they will each have a different regulation per minute.

Determine what type of fluid is in the new IV bag. The type of fluid will affect how often you need to change the patient’s IV. The normal lifespan of an IV solution without an additive is 72 hours, so after 72 hours, it will need to be changed. IV bags with additives need to be changed every 24 hours. As well, most IV bags with medications have a lifespan of 24 hours. IV solutions with additives have a shorter life span since the effectiveness of the additive or medication needs to be accounted for. IV bags with food substitutes like Lipid or TPN need to be changed every 24 hours, as just like solid food, these substitutes can go bad or spoil. If there are any TPNs and lipids left in the bag when you change it, they should be discarded. Keep in mind that regardless of what type of solution is in the IV bags, IV lines need to be changed every 24 hours. This prevents the tubing from clogging due to the different additives or TPN attached to the tubing.
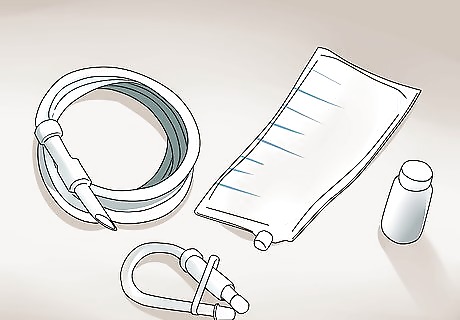
Prepare the necessary materials. These include: The prescribe IV fluid. Make the new prescribed IV fluid is available one hour before the procedure. Alcohol swabs or cotton balls with alcohol IV label IV pole/IV stand A watch with a second hand.

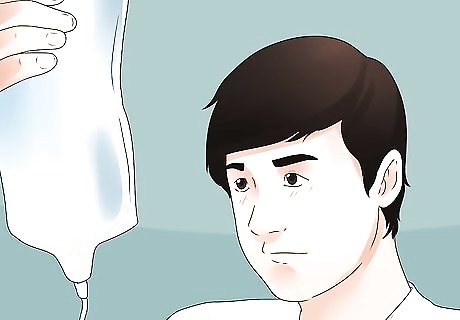
Check the sterility of the new IV infusion. The solution should be clear and there should be no matter in the solution. It should be sterile and in good condition. Also check for the expiration date of the solution. This is a vital check because there are risks associated with expired or unsterile fluids infused in patients.
Bring the necessary materials to the patient’s bedside. This will prevent any back and forth from another station to their bedside and save you time during the procedure.

Explain the procedure to the patient. This will lessen their anxiety and assure the patient cooperates. Inform the patient that you are going to replace the IV fluid and what type of fluid you are going to introduce into the patient’s system. Assure them that replacing the IV fluid does not mean you will need to reinsert the needle. Explain to the patient that they will experience a slight cold sensation when the fluid enters their veins, and that it will go away after 1-2 minutes.
Changing the Patient’s IV

Wash your hands thoroughly with anti-microbial soap and clean water. This will decrease the spread of microorganisms. Wet your hands and apply an anti-microbial soap. Rub your palms together. Continue to rub your palms together, as well as the back of your hands. Rub soap between the fingers on each hand and with your fingers together. Rub soap on both thumbs, in circles on both palms and on both wrists. Wash your hands for at least 20 seconds. A good way to estimate the right washing time is to sing the Happy Birthday Song twice. Once you’re done washing, rinse your hands, starting from the tip of the fingers to the wrist. Pat your hands dry with a clean cloth.
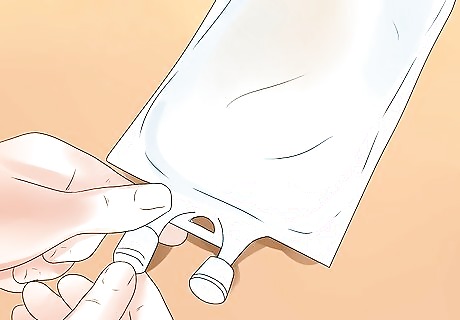
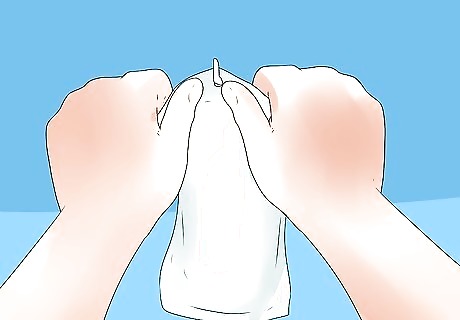
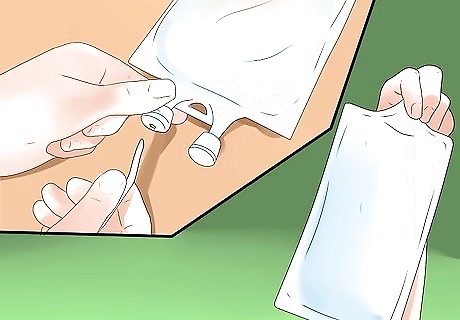
Prepare the new IV bottle. First, remove the cover of the IV bottle by pulling the plastic off the top of the IV fluid.

Disinfect the rubber port of the bottle. This is where you will insert the spike so it is important to this area by wiping the port with alcohol swabs or cotton with alcohol in a circular motion.
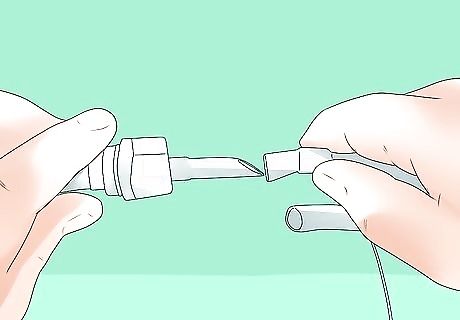
Close the roller clamp of the previous administration set by rolling it downwards. This will prevent liquid from leaking into the spike and a sudden gush of fluid from the new IV solution. The roller clamp is located in the long plastic tube, where the fluid runs from the IV.
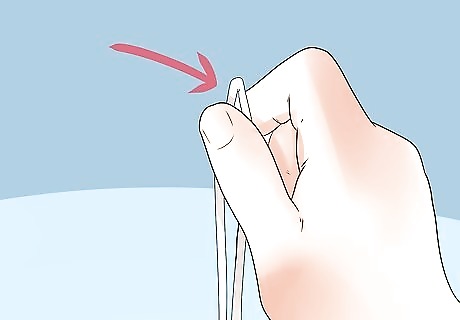
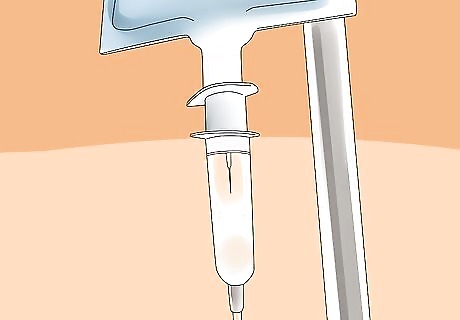
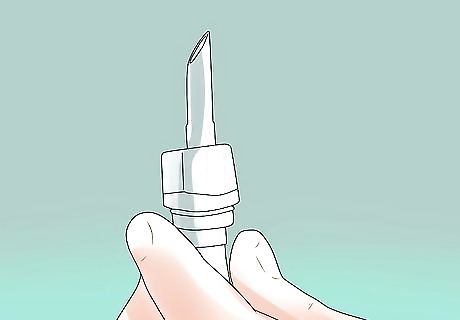
Kink the tubing of the administration set near the spike. Do this by folding the tube near the spike. This will prevent air from entering the tube. It is important that there is no air in the tubing because when air enters the body it will create an air embolus that can be very dangerous to the patient.
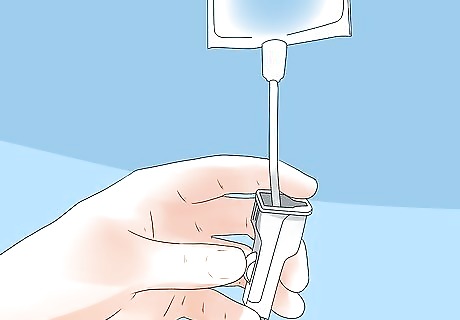
Spike the container without contaminating the port. Place the new IV fluid on a hard surface like the bedside table and firmly insert the spike until the end of the pointed part of the spike is completely inserted into the bottle. Avoid touching the spike, or letting it touch any other objects except the port, as this will prevent the spread of microorganism that can lead to infection.
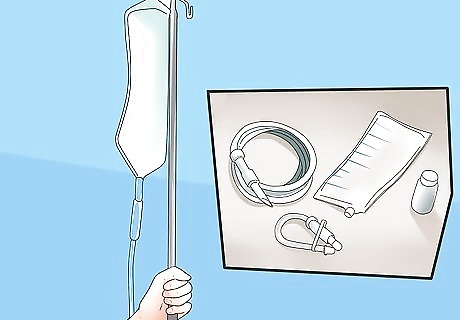
Hang the IV fluid on the designated IV pole. Make sure the pole is 2-3 feet taller than the patient to prevent a backflow of blood.
Regulate the flow rate based on the duration of the infusion. The flow rate or the drops per minute should be accurate to achieve the prescribed amount of fluid in the patient’s body. For example, if the prescribed flow rate is 42 drops per minute, use your watch to count the drops that accumulate in one minute. If the flow rate is too fast, move the roller of the roller clamp downwards. If the flow rate is too slow, move the roller of the roller clamp upwards. Then, count again until you reach the prescribe drops per minute.
Update the patient’s IV sheet. Include the type of solution, the type of medicine incorporated, the time and date the IV was changed, and the flow rate of the new IV solution.
Troubleshooting
If the IV fluid is close to the level of 100, change the IV. A level of 100 means the IV fluid is nearly empty, so be sure to change it before it runs out. Patients may also bring this to the attention of their nurse, as they will be able to observe if there is very little fluid left in the IV.
Allow the patient to go to the bathroom, sit in a chair, and move around the hospital room. Just make sure the patient has access to a help button or is within shouting distance of a nursing station or a hallway with medical workers. You want to be sure you are available if the patient needs help moving the IV pole or stand.
Check the IV regularly to make sure it is delivering the fluid correctly. As well, look for any blood in the tube, near the IV puncture site. This backflow is an indication you need to adjust the IV bottle so it hangs a little higher. As well, do not allow the patient to touch or adjust the roller clamp as only a qualified medical worker or nurse should adjust the IV’s flow rate.
If the patient complains of any pain or redness, check the needle. Pain and redness at the IV puncture site may indicate that the needle has dislodged from the vein.

















Comments
0 comment