views
Signs of Appendicitis

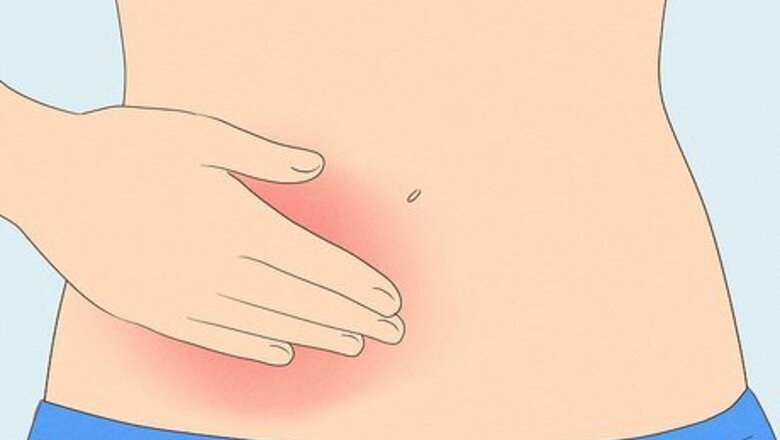
Pain in the lower right abdomen, fever, nausea, or decreased appetite The most common symptom of appendicitis is dull, persistent abdominal pain near the belly button that radiates or changes near the right lower belly. If you feel this discomfort, especially in addition to other symptoms, contact your doctor or go to the hospital as soon as you can. Delaying diagnosis will only make your appendix more likely to rupture and will endanger your life. You'll usually notice symptoms within 12 to 18 hours, but they may last up to a week, becoming more severe as time goes on. Other symptoms include: Decreased appetite Stomach problems like nausea, diarrhea, and constipation (especially if paired with frequent vomiting) A fever at or over 103°F (40°C). Go to a hospital immediately if your fever is this high, or if it's at 102°F (38°C) but you're experiencing several other symptoms. A low grade fever of around 99°F (37°C) Chills and shaking Back pain Inability to pass gas or feeling bloated The feeling that you need a bowel movement, even if your bowels are empty (known as tenesmus) If your pain comes and goes, you may have appendiceal colic, where severe cramping of the abdomen is caused by spasms or contractions of the appendix. The condition may eventually result in acute appendicitis.

Vomiting, painful urination, or pain in the back, rectum, or upper abdomen In addition to the symptoms above, you may also experience symptoms less commonly associated with appendicitis, like vomiting. If you suspect appendicitis, stay alert for symptoms like: Painful urination Vomiting before abdominal pain begins Sharp or dull pain in the rectum, back, or upper or lower abdomen
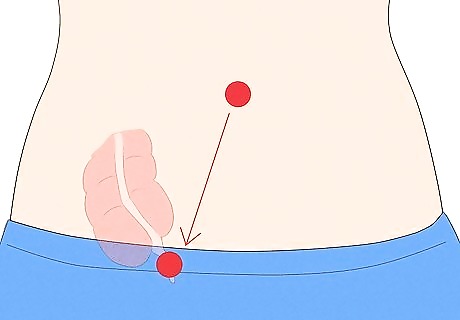
Pain that moves from your navel to your appendix In most adults, your appendix is located on the lower right side of your abdomen (usually one third of the way between your belly button and hip bone). Watch for a “path” of sharp pain—it might move from your navel (belly button) to the area directly over your appendix 12 to 24 hours after you start experiencing symptoms. If you've noticed a distinct progression like this, go straight to the emergency room. In adults, symptoms of appendicitis may get worse after as little as 4 hours. If you're diagnosed with appendicitis, it is considered a medical emergency. Note that the location of your appendix may be different for pregnant women.
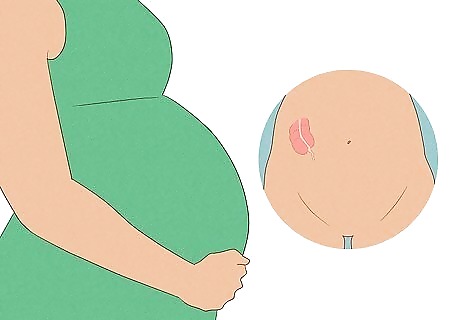
Vague abdominal pain (kids under 10, pregnant women, women over 50) It may be harder to detect appendicitis in pregnant women—the pain might be less severe and located higher in the abdomen because the appendix is displaced during pregnancy. In young children, the pain in the abdomen may be lower and accompanied by vomiting and/or swelling of the belly. Toddlers with appendicitis sometimes have trouble eating and may seem unusually sleepy (they may refuse to eat even their favorite snacks). In older children, pain typically starts at the belly button and moves to the lower right quadrant of the belly (like in adults). Pain does not get better if the child lies down, but may get worse if the child moves. A very high fever in a child could be a sign that the appendix is about to burst (or already has). Women over 50 may also experience vague or displaced abdominal pain, but this is rare. Typically, they will feel pain in the lower right abdomen like most adults.
Testing for Appendicitis at Home

Press on your abdomen to see if it’s painful to the touch. If it's too painful for you to even touch, especially in the lower right portion, consider going to the emergency room. Check yourself for rebound tenderness as well—press on your lower right abdomen and then quickly release your hand. If you feel a sharp pain, you may have appendicitis and need urgent medical attention. You may also feel a vague tenderness in your lower abdomen when you press on it. The most painful spot on your abdomen during appendicitis is called McBurney’s Point. It’s about two-thirds the distance from the navel to the bony projection of your right hip bone.
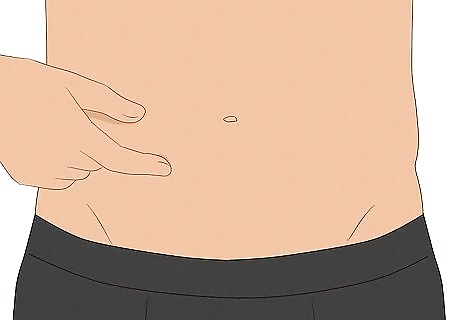
Poke your abdomen and note any firmness. When you press on your abdomen, is your finger able to sink in a bit? Or does your abdomen feel unusually firm and hard? If you notice the latter, you might be severely bloated, which is another symptom of appendicitis. Firmness or a hard mass in your abdomen may be a sign of peritonitis (an infection caused by a burst appendix). Visit the ER right away if the firmness is accompanied by pain. If you have abdominal pain, but don't have nausea or decreased appetite, it may not be appendicitis. There are many reasons for abdominal pain that don't need a visit to the emergency room. When in doubt, call or see your regular doctor for any abdominal pain that lasts more than 3 days.

Check for severe pain when you try to stand up straight and walk. If you can't do this without severe pain, you might have appendicitis. Seek emergency care immediately, and ease your pain or discomfort by lying on your side and curling into the fetal position. See if your pain gets worse if you make jarring movements or cough. This could be another indication of appendicitis.
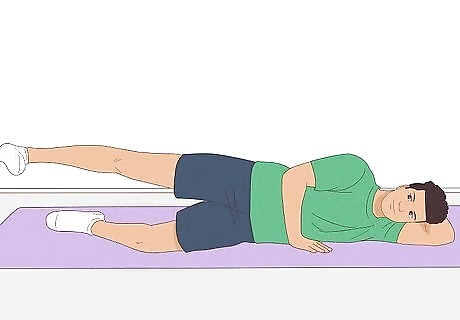
Test for sharp abdominal pain when you flex your right hip. Lie down on your left side, then try to extend your right hip. If your pain stays the same or worsens (or if you’re unsure), contact your healthcare provider right away. Alternatively, try flexing your right hip and knee or rotating your hip from any position and feel for similar sharp, worsening, or persistent pain. This test is not a certain indicator of appendicitis. However, it may help a doctor diagnose whether you have appendicitis or not.
Getting a Diagnosis
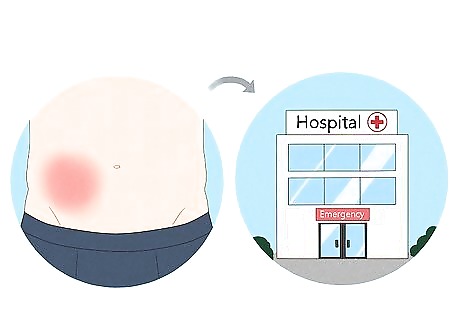
Get to an emergency room immediately for appendicitis symptoms. If you feel reasonably certain you have appendicitis, go to a hospital as soon as possible rather than making a doctor's appointment for a later time. Appendicitis is potentially life-threatening if the appendix bursts without treatment. Pack some overnight items, such as fresh pajamas and your toothbrush. If you have appendicitis, you'll be getting surgery and staying overnight. Do not take any pain medication or laxatives before heading to the ER, as these can exacerbate your symptoms. Avoid eating and drinking since these may complicate surgery.

Explain your symptoms at the emergency room. Be prepared for triage and tell the triage nurse that you suspect appendicitis. Mention all of the symptoms you noticed in detail, including where and when you felt pain, how severe the pain feels, and any other symptoms you had. You'll then be ranked on a list of patients who need care according to the immediacy of their injuries. If you have time or aren’t incapacitated by pain, write down a quick summary of your symptoms and any medications you take and request copies be included in all reports during your visit. Don't panic if you have to wait—you're a lot safer at the hospital than at home. Try to be patient and take your mind off the pain by distracting yourself with a book or your phone, or conversing with any friends or family who accompanied you.

Communicate your symptoms to a doctor during a physical exam. When you get to see a doctor, describe your symptoms again. Note any digestive abnormalities (such as constipation or vomiting), and try to tell the doctor when you first noticed the pain. The doctor will then physically examine you for signs of appendicitis. Expect your abdomen to be prodded. The doctor will press hard on your lower abdomen to check for peritonitis (the infection that results from a burst appendix). If you have peritonitis, your abdominal muscles will spasm when pressed and may feel painful. The doctor might also perform a rectal exam, depending on your symptoms and their severity.
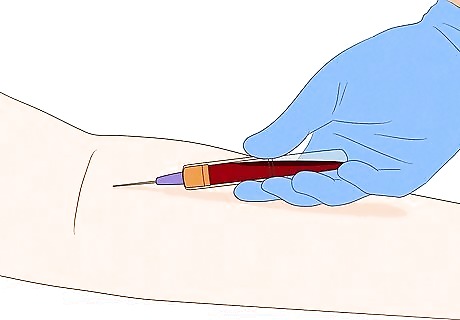
Expect additional lab tests. Lab testing and imaging are important for the official diagnosis of appendicitis, since physical exams cannot show what’s happening inside your body. Lab testing is often painless and doesn’t require any preparation unless you’re instructed not to eat or drink prior to an imaging test. Possible tests include: Blood test: This will identify a high white blood cell count, which signifies an infection (even before a low-grade temperature is seen). The blood test will also show if there is an imbalance of electrolytes or dehydration, which can cause pain as well. The doctor may also run a pregnancy test for women. Urinalysis: A urine test will show a possible urinary tract infection or kidney stone, which may also present with appendicitis-like abdominal pain at times. Ultrasound: An ultrasound of the abdomen will show if there is a blockage, rupture, or swelling of the appendix (or another reason for the abdominal pain). Ultrasounds are usually the first resort for imaging. MRI: MRI (magnetic resonance imaging) tests are used to get a more detailed picture of the internal organs without using an x-ray. It will show the same signs as an ultrasound, but in more detail. Expect to feel slightly claustrophobic in the MRI machine. Your physician may order light sedation to help ease the anxiety. CT Scan: CT (computed tomography) scans use an x-ray with computer technology to show images. You may be given a solution to drink that will “dye” your veins for better imaging. This test will show signs of inflammation, bursting, or blockage of the appendix.
Treatment & Recovery

Avoid pain medications until you get medical treatment. If you have symptoms of appendicitis, then certain medicines may make your symptoms worse as you wait for treatment in the emergency room. Avoid the following over-the-counter medications or pain management techniques: Pain medication: Pain medication can make it harder for you to monitor and track any spikes in abdominal pain. Laxatives: Laxatives might irritate your intestines further and cause more discomfort or pain. Antacids: Antacids can worsen pain associated with appendicitis. Heating pads: Heating pads might cause an inflamed appendix to rupture. Food or drink: Don't eat or drink anything until you've been examined, because this can make you a higher risk for aspiration during surgery.
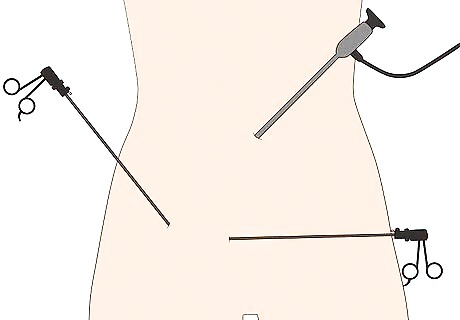
Get an appendectomy to remove an infected appendix. If your doctor determines that you do have appendicitis, the only cure is to remove the appendix in a surgery called an appendectomy. Most surgeons prefer a laparoscopic procedure, which is minimally invasive and leaves less of a scar than an open appendectomy. If your doctor does not think you need surgery, they may send you home to be “on watch” for 12 to 24 hours. During that time, do not take antibiotics, pain medicine, or laxatives, and contact your provider if you get worse. When you return, make sure not to eat or drink anything in advance because this could cause complications in surgery. Appendectomies are safe, commonplace procedures with low complication rates if they’re performed before the appendix ruptures. If the appendix has burst, the risk of complications is about 25%.
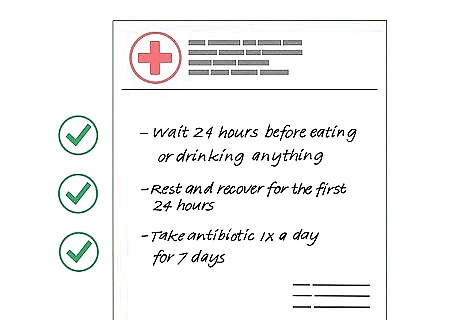
Follow your doctor’s recovery instructions over the next 2-4 weeks. Modern appendectomies are minimally invasive, and you’re likely to leave the hospital in 1-2 days and return to normal life with few to no complications within 2-4 weeks. However, surgery is taxing no matter how successful the procedure is, so follow your provider’s post-operation recovery regimen closely. Wait 24 hours before eating or drinking anything. Your doctor will tell you when you can have small amounts of liquids, then solid foods. Rest and recover for the first 24 hours. Try to engage in light activity and movement, like walking, over the following few days and avoid strenuous lifting or high-impact activities, like running. Take any prescribed antibiotics. If your appendix burst before surgery, you will likely be given an oral or intravenous antibiotic to take during recovery to prevent infection. Call your doctor if you notice problems including pain, vomiting, dizziness, faintness, fever, diarrhea, bloody urine or stool, constipation, drainage or swelling around the incision site, or lingering symptoms of appendicitis.

















Comments
0 comment