
views
X
Trustworthy Source
Mayo Clinic
Educational website from one of the world's leading hospitals
Go to source
CPR usually involves a combination of chest compressions and rescue breathing, but the exact method and duration varies depending on the situation and who the victim is. If you’re not trained in performing CPR, many health experts recommend doing hands-only CPR, which doesn’t involve rescue breaths.[2]
X
Trustworthy Source
Harvard Medical School
Harvard Medical School's Educational Site for the Public
Go to source
CPR can be performed on adults, children, infants, and even most pets.
Using Hands-Only CPR for Adults and Teens
Examine the scene for any obvious hazards. In some cases, it may not be safe to perform CPR. If there are any dangers nearby preventing you from getting close to the person, don’t endanger your own life as well as theirs. Call emergency services and wait for help to arrive. For example, if the person has collapsed due to exposure to smoke and fire or toxic fumes, steer clear of the area. If the person is in a dangerous situation and you’re able to move them safely, do so before trying to give them CPR. For example, if they’ve collapsed in the middle of the street, wait for a moment when there’s no oncoming traffic and then move them out of the road.

Check for unresponsiveness. If an adult or teen collapses but remains conscious, CPR is not typically needed. If they lose consciousness and are not breathing, however, you should administer rescue breaths if possible, or stick to hands-only CPR if you’re not trained in doing rescue breathing. If they’re not breathing, have no pulse, and are unresponsive, try to perform some form of CPR even if you are untrained or rusty in your abilities. Shake the victim's shoulders and loudly ask, "Are you okay?" If you receive no response, check for signs of breathing, like the person’s chest rising and falling. Check for a pulse by placing your fingers on their carotid artery, next to the windpipe just below the jaw. Hands-only CPR is ideal for those without formal CPR training or for people unsure in their CPR abilities. It does not involve the rescue breathing measures associated with conventional CPR, but instead focuses on chest compressions.

Call the Emergency Services. If you find a person who is unresponsive, isn’t breathing, or doesn’t have a pulse and you decide to do some form of CPR, you should still immediately call your local emergency number before you do anything else. CPR can revive people on occasion, but it should be viewed as buying time until emergency personnel arrive with appropriate equipment. If 2 or more people are available, 1 person should dial for help while the other begins CPR. If a person is unresponsive because of suffocation (from drowning, for example), then it's recommended to immediately begin CPR for 1 minute and then call your local emergency number. If the victim is a child between the ages of 1 to 8 years, perform 5 cycles of chest compressions and rescue breathing before calling emergency services if you are the only person available. This should take roughly 2 minutes. Calling emergency services will bring paramedics to the location. Typically, the dispatcher will also be able to instruct you on how to perform CPR.
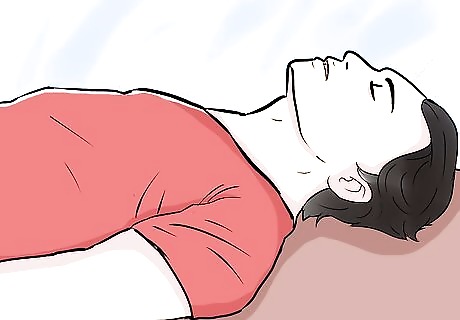
Keep the victim on their back. In order to perform hands-only CPR, the victim should be positioned on their back (supine), preferably on a firm surface, with the head facing up. If the person is on their side or stomach (prone), then gently roll them onto their back while trying to support their head and neck. Try to make note if the person experienced significant trauma while falling and becoming unconscious. Once on the person is on their back, kneel next to their neck and shoulders so you have better access to their chest and mouth. Keep in mind that you should not move the person if you suspect they may have suffered a significant head, neck, or spinal injury. In this case, moving them is life-threatening and should be avoided, unless emergency help won't be available for a long time (a few hours or more).
Tilt the person’s chin up to open their airway. Once you have them on their back, tilt their head back while pressing their chin up and forward with 2 fingers. This should move their tongue out of the way and make it easier for them to breathe. If you’re afraid the person has a neck injury, try not to move their head. Use both hands to carefully move their jaw forward without moving the rest of their head or neck. Once you’ve opened the airway, listen carefully for sounds of breathing and check to see if their chest is rising and falling. If you can’t find any signs of breathing after about 10 seconds, or if the person is only gasping occasionally instead of breathing regularly, start CPR.

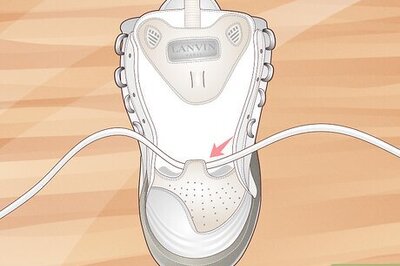
Rapidly push down on the center of the chest. Place one hand directly over the center of the person's chest (between their nipples, generally) and your other hand on top of the first for reinforcement. Press down on the victim's chest firmly and quickly—aim for about 100 chest compressions a minute until paramedics arrive. If you're not sure what 100 compressions a minute really means, try doing your compressions to the beat of the Bee Gee's song "Stayin' Alive", or Queen's song '"Another One Bites the Dust". Use your upper body weight and strength, not just your arm strength, to push straight down on the chest. Your chest compressions should cause the person's chest to depress at least 2 inches (5.1 cm). Push hard and understand that it is likely you will break the person's ribs. This is extremely common, and you shouldn't stop compressions even if you think this has happened. Chest compressions are hard work and you may have to switch off with other bystanders before emergency personnel arrive. Continue doing this action as until the person becomes responsive or until the emergency medical team arrive and take over.
Using Conventional CPR for Adults and Children

Follow the same initial procedures as hands-only CPR. Even if you have recent CPR training and are confident of your abilities, you still need to assess the person to see if they are responsive. Move them onto their back if they are not responsive and show no sign of neck, head, or spine injury. Try to call emergency services before starting chest compressions and look for someone to trade off with. If performing CPR on a small child between the ages of 1 and 8 years, only use 1 hand to perform chest compressions. The rate of chest compressions is the same for both adults and children (roughly 100 per minute). For children between the ages of 1 and 8 years, you will need to depress the sternum (chest bone) 1/3 to 1/2 of the depth of the child's chest. If you have recent CPR training, perform only 30 chest compressions before moving on to the breathing assistance phase of CPR.

Proceed to open the airway. If you're trained in CPR, confident of your abilities (not rusty), and you've performed 30 chest compressions, then proceed to open the person's airway using the head-tilt, chin-lift technique, or the jaw-thrust if you suspect a neck/head/spine injury. Put your palm on their forehead and gently tilt (extend) their head back a little. Then, with your other hand, gently lift the chin forward to open up their airway, making it easier to give them oxygen. Take 5 to 10 seconds to check for normal breathing. Look for chest motion, listen for breathing, and see if you can feel the victim's breath on your cheek or ear. Note that gasping is not considered to be normal breathing. If they are already breathing, no breathing assistance is needed. However, if they are still not breathing, then proceed to the mouth-to-mouth breathing part of CPR. To perform the jaw-thrust technique, sit above the person's head. Place one hand on each side of the person's jaw and lift the jaw so that it is jutting forward, as though the person has an underbite.

Place your mouth over the victim's mouth. Once the person's head is tilted and their chin lifted, make sure their mouth is free of any objects blocking their airway. Then, use one hand to pinch the victim's nostrils closed and cover their mouth completely with your own mouth. Form a seal with your mouth so that no air can escape while you attempt to give the victim a rescue breath. You should be aware that mouth-to-mouth CPR can transfer infectious viral and bacterial diseases between the victim and the rescuer. Before contacting their mouth with yours, wipe away any vomit, mucus, or excess saliva that may be present. Rescue breathing can also be mouth-to-nose breathing if the person's mouth is seriously injured or can't be opened.

Start with 2 rescue breaths. Once your mouth is over the other person's, forcefully breathe into their mouth for at least 1 full second and watch their chest to determine if it rises a little or not. If it does, give the second breath. If it doesn't, then repeat the head-tilt, chin-lift maneuver and try again. Don't be too timid or grossed out, because a person's life is in your hands. Although there's carbon dioxide in your breath when you exhale, there's still enough oxygen to benefit a victim during CPR. Again, the purpose isn't always to revive them or continue indefinitely, but to buy some time for them until paramedics arrive. Approximately 30 chest compressions and 2 rescue breaths is considered to be 1 cycle of conventional CPR for both adults and children. If performing CPR on a child between the ages of 1 and 8 years, you can use gentler breaths to inflate their lungs.

Repeat cycles as needed. Follow the 2 rescue breaths with another round of 30 chest compressions and 2 more rescue breaths. Repeat as needed until the victim becomes responsive or until emergency medical personnel can take over. Remember that chest compressions attempt to restore some sort of circulation, while the rescue breathing provides some (but not much) oxygen to prevent tissues, particularly the brain, from dying.
Using CPR for Infants (Under 1 Year)

Assess the situation to figure out if their airway is blocked. The most common cause of infant suffocation is choking. You need to assess the situation to determine if the airway is completely blocked or only partially blocked. If the baby is coughing or gagging, the airway is partially blocked. Let the baby continue to cough, as this is the best way to dislodge the blockage. If the baby is not able to cough and begins to turn bright red or blue, the airway is completely blocked. You will need to perform back blows and chest compressions to dislodge the blockage. If your baby is ill, having an allergic reaction, or suffocating because their airway is swollen, you can perform chest compressions and rescue breaths, but you will need to call local emergency services immediately.
Position the baby between your forearms. Position the baby so that they are face-up on 1 forearm. Cradle the back of their head with the hand of the same forearm. Place your other forearm over the baby's front and gently turn them over so that they are face-down, remaining sandwiched in between your arms the entire time. Use your thumb and fingers to hold the jaw as you turn the baby. Lower your bottom arm onto your thigh. The baby's head should be lower than their chest. Note that back blows should only be delivered if the baby is still conscious. If the baby falls unconscious, skip the back blows and proceed straight to the chest compressions and rescue breaths.

Deliver back blows to dislodge an airway obstruction. Use the heel of your dominant hand to deliver 5 gentle yet distinct back blows in between the baby's shoulder blades. Continue to support the baby's neck and head by holding their jaw between your thumb and forefingers. Giving CPR to a baby is often walking a fine line between being effective and causing injury. However, a minor musculoskeletal injury is a small price to pay for saving a life.

Place the baby on their back. After delivering the gentle back blows, place your free hand on the back of the baby's head, resting your arm firmly along the baby's spine. Carefully turn the baby back over so they are face-up again. Don't lift the baby's head as you turn them, as this can force the clog back into their throat. Keep the head down. The baby should remain sandwiched in between your arms as you turn them. Remember to remain calm and talk soothingly to the baby. They can't comprehend your words, but they can pick up on your calm and loving tone.

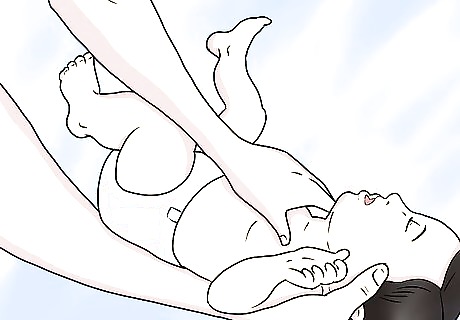
Position your fingers in the center of the baby's chest. Position the tips of 2 or 3 fingers in the center of the baby's chest while supporting the baby's neck and head with your other hand. Use your thumb and fingers to hold the jaw as you sandwich the baby in between your forearms. The lower arm should support the baby's back on your opposite thigh, and the baby's head should be lower than the rest of their body. You could also place the baby on their back on a firm, flat surface, like a table or the floor. The fingers should be placed in between the baby's nipples at the center of their chest.
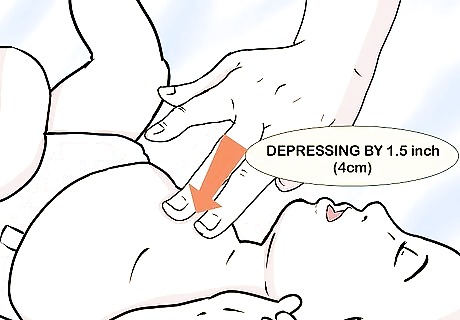
Gently compress the chest. Push straight down on the chest, depressing it by about 1.5 inches (3.8 cm). If the baby is conscious, only perform 5 compressions. If the baby is unconscious, perform 30 compressions. Pump rapidly at a rate of 100 compressions per minute. Each compression should be smooth, not abrupt or shaky. Be careful not to injure the baby's ribs during the compressions.

Cover the baby's nose and mouth and breathe. You do not need to pinch the nose plugged as you would do with an adult. Instead, seal off the baby's breathing passages by placing your entire mouth over their nose and mouth. Make sure to wipe away any vomit, blood, mucus, or saliva first. Give 2 gentle rescue breaths. Deliver 1 puff of air into the baby's mouth. If the chest moves, deliver the second puff of air. If the chest does not move, attempt to clear the airway again before administering the second breath. Do not deliver deep breaths of air from your lungs. Instead, use the muscles in your cheeks to deliver gentle puffs of air.
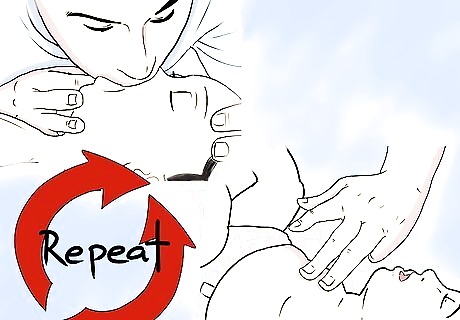
Repeat the cycle as needed. Repeat chest compressions and rescue breaths as needed until the baby begins to breathe again or until emergency medical professionals arrive. If you suspect that the baby is choking on a foreign object, you should look into their mouth after every round of chest compressions. Each cycle should consist of 30 chest compressions followed by 2 emergency breaths.















Comments
0 comment