
views
X
Research source
If done improperly, air could leak back into the pleural space (the space between the lungs and the chest cavity) and the lung could collapse again.[2]
X
Research source
Chest tubes are inserted to drain pus, blood, or air that builds up in pleural space.[3]
X
Trustworthy Source
MedlinePlus
Collection of medical information sourced from the US National Library of Medicine
Go to source
These substances build-up due to surgery, illness, or injury and can inhibit normal breathing function by partially or fully collapsing the lung. Chest tubes are removed when there is no more air or fluid to drain from the pleural space. The site should heal over within a couple of weeks and leave a small scar.[4]
X
Research source
The following contains an overview of the procedure for removing chest tubes, intended as an informal refresher for medical professionals.
Note: The steps in part 2 (removing the chest tube) must be done in rapid succession. Make sure to read over and completely understand part 2 in advance.
WARNING: Do not attempt to remove a chest tube unless you are a qualified medical professional.
Preparing for Removal
Decide if it is time for removal. A medical professional will decide when it is time for a chest tube to be taken out. The following is a list of factors to consider. The chest tube has been used for about a week. Long use of chest tubes can increase the chance of infection. The amount of fluid drained has decreased substantially, usually to less than 200 mL 24 hours. Respiration has returned to normal. The patient is no longer short of breath, the breathing rate has returned to normal, and the chest rises symmetrically upon air intake. X-rays (or other tests) show an absence of air or fluid in the pleural cavity.

Explain the procedure to the patient. It is important that the patient understands what he will need to do during the procedure, such as the Valsalva maneuver. The patient may also be nervous about pain. They will remember the pain of insertion (if they were conscious), and chest tubes can also be quite painful while inserted. It will be important to reassure the patient, as the removal of a chest tube is usually less painful than going in.
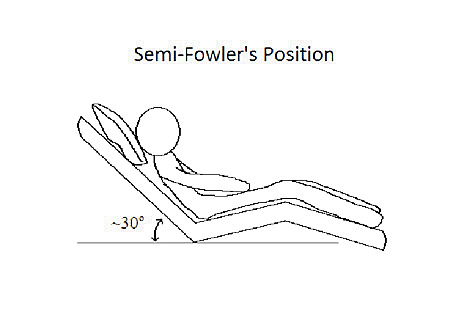
Position the patient in a semi-Fowler's position. Lay the patient on his back and elevate the head of the bed by a small amount (usually about 30). The patient's knees may be flat or may be elevated by a small amount. The patient's arms should be relaxed and out of the way.
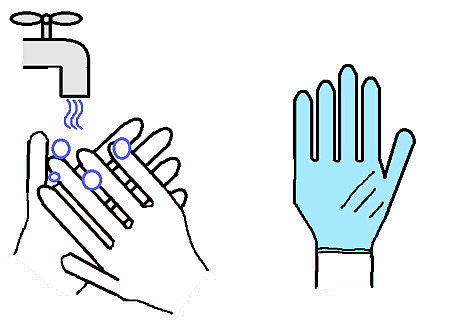
Wash your hands and put on gloves. Washing your hands and wearing gloves are critically important in reducing the chance of spreading diseases such as infection. Warning: Use latex-free gloves if the patent is allergic to latex.
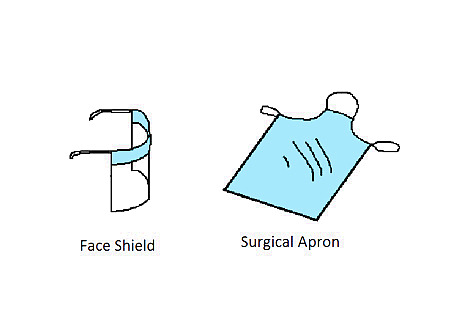
Put on an apron and face shield. This is done to protect yourself from any splatter or drainage, as removing a chest tube can be a messy procedure. A face shield consists of a clear, plastic panel that straps around the forehead and covers the face. A surgery apron is a thin plastic gown that straps around the chest and covers the upper half of the body.
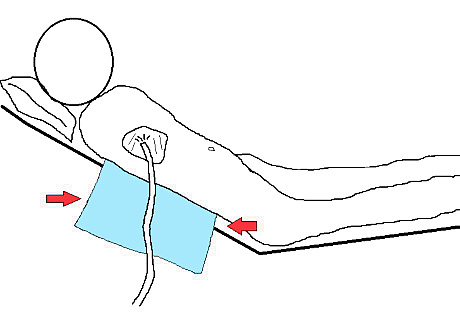
Place a pad to collect drainage. A pad will protect the surroundings from drainage. Disposable pads often contain an absorbent fabric layer (to soak up liquid) and a plastic layer (to protect the covered surfaces). The plastic layer should go down. Several pads may be needed.
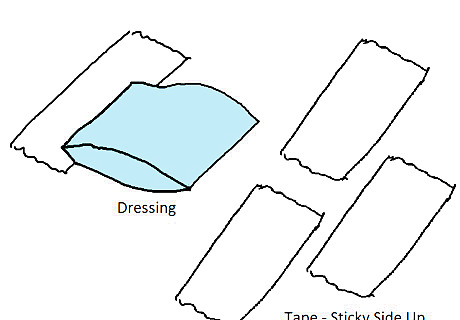
Prepare a new dressing and tape for easy placement. Attach a single piece of tape to a prepared dressing and lay it in a convenient location. Also have strips of tape ready to use and lay them sticky-side up. Having the dressing ready to use will reduce the time it takes to cover the hole after the chest tube is removed. The hole must be sealed quickly to keep air from entering the pleural space, which could cause the lung to collapse.
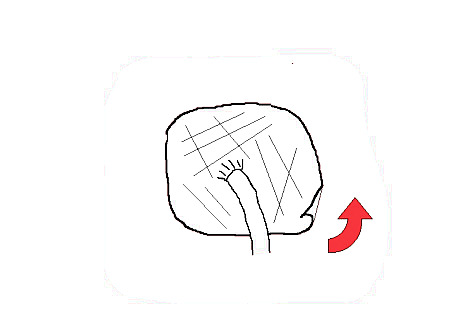
Remove the chest tube dressing carefully. Make sure to avoid tugging on the chest tube. The dressing usually consists of a soft bulky interior (to seal and protect the area) and tape around the edges. Peeling away the tape from several sides will release the dressing gently.
Change gloves after removing the dressing. This is done to maintain a sterile environment, as the old gloves are contaminated from removing the dressing.
Removing the Chest Tube
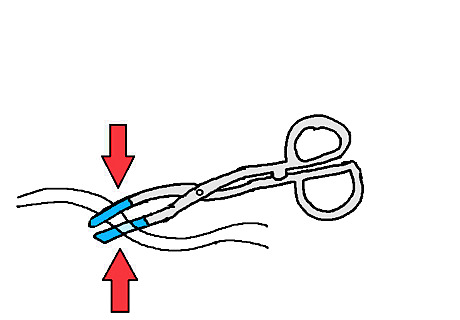
Clamp the tube using a rubber-tipped Kelly clamp, and discontinue suction. This is to stop any air flow from entering or leaving the pleural space. The rubber tips help prevent damage to the chest tube. The Kelly clamp also locks itself in place using a gripping mechanism near the handles.
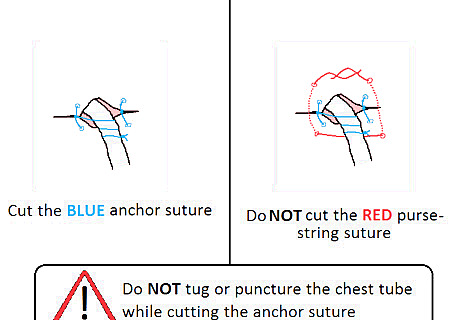
Cut the anchor suture that holds the tube in place. Warning: Do not puncture or cut the chest tube. The change in air pressure could cause the lungs to collapse. Warning: Make sure to hold the chest tube in place after the anchor suture has been cut, as there is nothing left holding the tube in place. Warning: If present, do not cut the purse-string suture. Some doctors prefer to include a purse-string suture when inserting the chest tube, for the purpose of closing the site once the tube has been removed.
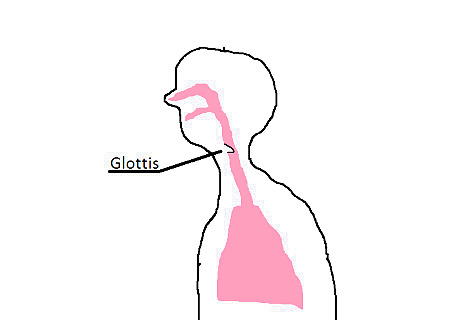
Instruct the patient to perform the Valsalva maneuver. To perform the maneuver, have the patient take a deep breath. Then the patient should close the back of the throat (the glottis or windpipe) and attempt to force air through it. The maneuver decreases the chance of the lungs collapsing as the chest tube is removed. The patent can alternately, instead of closing the back of the throat, hold the nose and mouth closed.
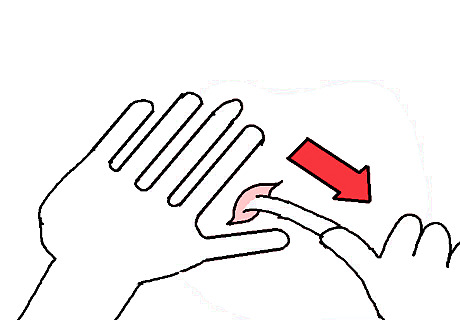
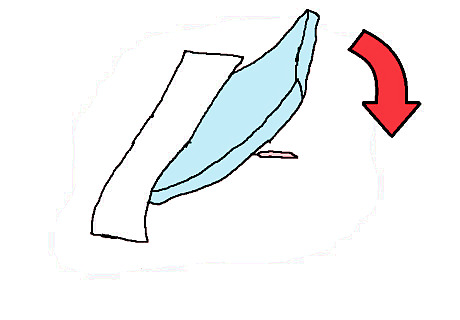
Remove the tube swiftly and gently while the patent is performing the Valsalva maneuver. Place one hand gently around the site and use the other to carefully remove the tube. Some fluid leakage and spray are normal. Be prepared for the following steps, as the site must be sealed as soon as possible.
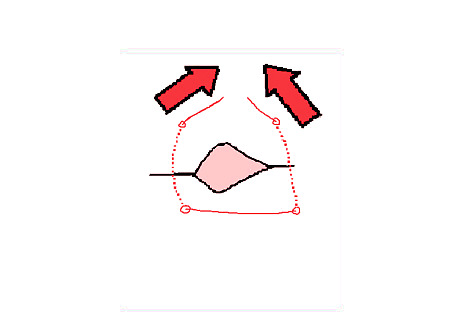
Close the purse-string suture immediately, if present, and observe the site for escaping air. It may be necessary to have a second pair of hands to close the suture quickly. As the suture is tightened, the hole closes and prevents air from entering. The site should be examined for bubbling, which indicates airflow.
Cover the site immediately with an appropriate dressing. Several different kinds of dressing can be used (such as an occlusive dressing). The dressing used often depends on the facility performing the procedure. In all cases, the dressing should seal off the site to prevent the entry of any air.
Providing Care Afterwards
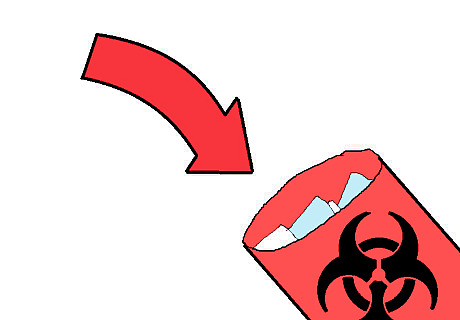
Dispose of waste properly. Double bag the chest tube, disposable pad, and any other supplies that were contaminated during the procedure. Warning: Avoid contact with medical waste. Blood and other bodily fluids can transmit diseases.
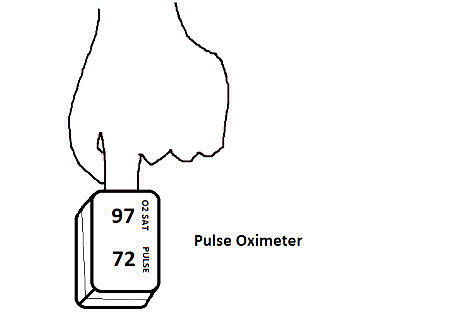
Monitor the patent’s respiratory condition. Look for: Low blood oxygen saturation (measured using a pulse oximeter). Persistent bleeding. Chest discomfort. Shortness of breath. Signs of infection.
Perform an x-ray to make sure the lung is properly functioning. An x-ray can indicate if fluid has again built up in the pleural space. It may be necessary to perform another x-ray at a later date.














Comments
0 comment