views
X
Expert Source
Kevin Stone, MDBoard Certified Orthopaedic Surgeon
Expert Interview. 19 November 2020.
Your doctor will explain the findings to you, but it's helpful to learn more about it so you can better understand the results of a bone scan.
Interpreting Bone Scans
Get a copy of your bone scan. A doctor who specializes in reading bone scans (radiologist) will send their interpretation of your results to your family doctor who will then explain them to you — hopefully, in simple terms. If you want to take a closer look, you can ask to see the original scan at your doctor's office or ask for a copy to take home. Although your doctor will likely be reluctant to give you the original bone scan to take home, he must legally provide you with a copy if you ask. The office might charge you a small copying fee. A bone scan is done to show problems with bone metabolism — the process of building and recycling bone tissue. Some activity is normal, but too much or too little bone remodeling is a sign of disease or injury.
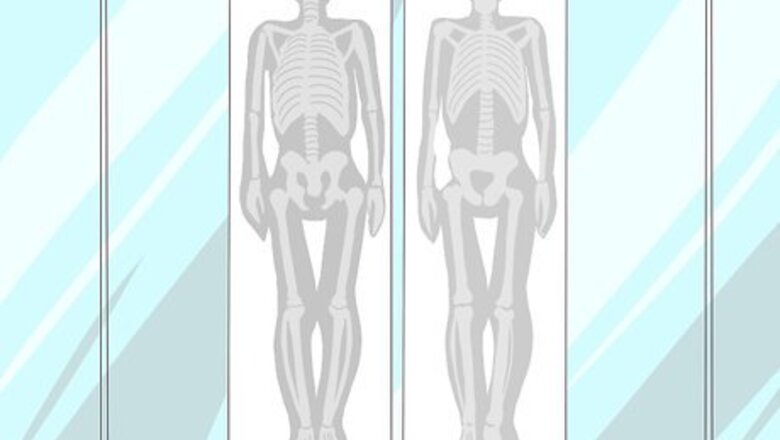
Identify the bones in your scan. Most bone scans take an image of the entire skeleton, but sometimes they're more focused on an injured or painful area, such as the wrist or spine. As such, learn a little about basic anatomy, especially the names of most of the bones in your bone scan. Search online for information or borrow a book from your local library. You don't need to learn detailed physiology or anatomy, but you should know what bones the radiologist is referring to in her written report of your bone scan results. The most common bones that are noted on bone scans are the vertebrae (spinal bones), pelvis (ilium, ischium, and pubis), ribs, wrists (carpal bones), and leg bones (femur and tibia).
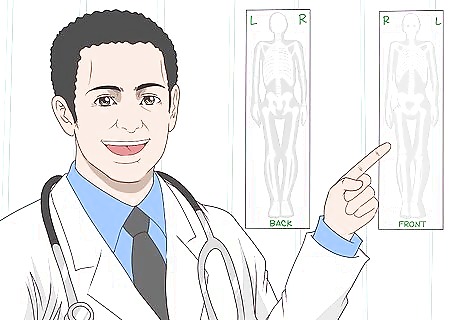
Get properly orientated. Once you have an idea of the bones that are problematic on your bone scan, you also need to know on which side of your body it is. You often can't tell just by looking at your body image, but all diagnostic images including bones scans have to be labelled in terms of which side is the patient's right and which is left. As such, look for words such as left, right, front or back on the image to get orientated. Bone scan images can be taken from either your front or back. Looking at the head, you can sometimes see from which direction it was taken, but not always. Instead of words, bone scans and other diagnostics images may be orientated by marker letters, such as L (left), R (right), F (front), or B (back).
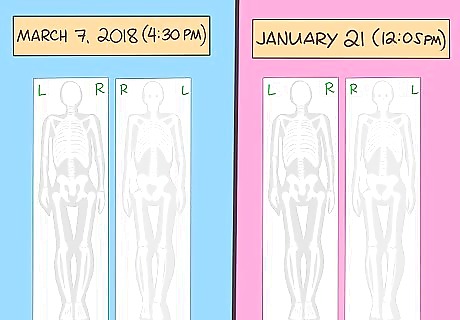
Determine the time frame. If you have more than one bone scan taken over time, which is common when following the progression of a bone disease or condition, then determine the dates (and times) that each was taken by looking at the label. Study the earlier one first, then compare it to later ones and take note of all the changes. If there isn't much difference, then it's likely your condition hasn't progressed (or improved). If you have osteoporosis, for example, your doctor will likely recommend a yearly or bi-yearly bone scan to monitor progression of the disease. If a bone infection is suspected, images may be taken shortly after the radio-tracer is injected into you and again three to four hours later when it's collected in your bones — this is called a 3-phase bone scan.
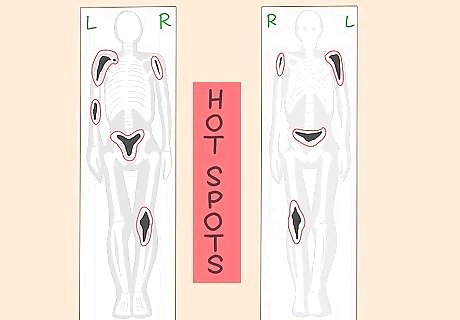
Look for "hot spots." The test results of a bone scan are considered normal when the radioactive dye is spread and absorbed evenly throughout your skeleton; however, a bone scan is considered abnormal when it shows darker colored "hot spots" in your bones. Hot spots show areas in your skeleton where an excess of dye accumulates, which could signify bone destruction, inflammation, fractures or tumor growth. Diseases that cause bone destruction include aggressive types of cancer, bacterial bone infection, and osteoporosis (leads to weakening and fractures). Some bones can normally appear slightly darker than other bones because of their increased metabolic activity. Examples include your sternum (breastbone) and parts of your pelvis. Don't mistake these for diseases. In some cases, as with lesions resulting from multiple myeloma, hot spots will not appear on a bone scan. A CT or PET scan may be more helpful to identify signs of this type of cancer.
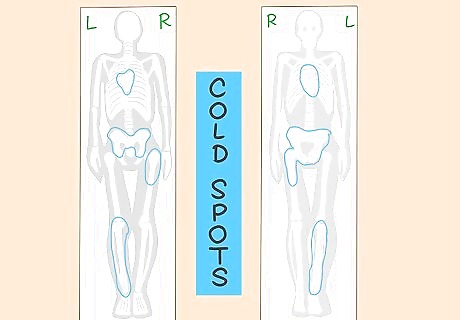
Look for "cold spots." Test results are also considered abnormal when there are lighter colored "cold spots" in your bones. Cold spots indicate areas that absorb less radioactive dye (or none) compared to surrounding bones due to reduced activity and remodeling. In general, cold spots are usually a sign of decreased blood flow to an area for some reason. Lytic lesions — associated with multiple myeloma, bone cysts, and certain bone infections — may show up as cold spots. Cold spots can indicate poor circulation due to a blood vessel blockage (atherosclerosis) or benign tumor. Cold spots and hot spots can appear simultaneously on a bone scan and represent different but concurrent diseases or conditions. Although lighter cold spots are abnormal, they typically represent conditions that are less serious than those represented by darker hot spots.

Understand the results. The radiologist will interpret your bone scan results and send a report to your doctor, who will use that information along with other diagnostic studies and/or blood tests to establish a diagnosis. Common diagnoses that stem from abnormal bone scan results include: osteoporosis, bone fractures, bone cancer, bone infection, arthritis, Paget's disease (a bone disorder involving thickening and softening of bones) and avascular necrosis (death of bone due to lack of blood supply. With the notable exception of avascular necrosis, which shows up as cold spots on a bone scan, all the other above-mentioned conditions show up as hot spots. Common osteoporosis hot spots to see on a bone scan include the upper thoracic spine (mid-back), the hip joints and/or the wrists. Osteoporosis leads to fractures and bone pain. Cancer hot spots can be seen in virtually any bone. Bone cancer often spreads (metastasizes) from other cancer sites, such as the breasts, lungs, liver, pancreas, and prostate gland. Paget's disease causes hot spots along the spine, pelvis, long bones and skull. Bone infections are most common in the leg, feet, hand, and arm bones.
Preparing for a Bone Scan

Remove jewelry and other metal objects. Although you don't need to make any special preparations before taking a bone scan, you should dress in comfortable, easily removed clothes and refrain from wearing any jewelry. Metal jewelry and watches, in particular, should be left at home or removed just prior to the bone scan because they can affect the results. Like other diagnostic imaging tests, such as x-rays, any metal on your body will make the bone scan images look white or lighter than surrounding areas. Tell the radiologist and/or technician if you have any metal fillings in your mouth or metal implants in your body, so they can make note of it and not confuse them with disease processes. Wearing clothes that are easily removed is a good idea because you may be asked to wear a hospital gown.
Tell your doctor if you are pregnant. Inform your doctor if your pregnant or potentially pregnant because the radiation exposure from the radiotracer can be harmful to the baby. As such, bone scans aren't often performed on pregnant people or nursing mothers — the breast milk can become slightly radioactive and harm the baby also. There are other imaging tests for bone that are safer for pregnant people, such as MRI studies and diagnostic ultrasound. Short-term osteoporosis is not uncommon with pregnant people who are malnourished because minerals are leached from their bones to provide for the growing baby.

Don't take any medicine containing bismuth. Although you can eat and drink normally just prior to your bone scan, tell your doctor about the medications you're taking, as these may affect your test. For example, medicines that contain barium or bismuth affect bone scan test results, so you should avoid taking them for at least four days prior to your appointment. Bismuth is found in a variety of medicinal products, such as Pepto-Bismol, Kaopectate, Devrom, and De-Nol. Bismuth and barium can cause areas of your body to look too light on bone scans
Understanding the Risks
Understand the radiation risk. The amount of radiotracer injected into your vein just prior to getting a bone scan is not very much, but it still produces radiation in your body for up to 3 days. Radiation increases the risk of healthy cells mutating into cancer cells, so make sure you weigh all the pros and cons with your doctor before getting a bone scan. It's estimated that a bone scan exposes you to no more radiation than a conventional full-body x-ray does and less than half that of a CT scan. Drinking lots of water and fluids starting immediately after a bone scan for 48 hours can help to flush out any radioactive tracer left in your body. If you must have a bone scan while breastfeeding, pump and throw away your breast milk for two to three days so your baby isn't harmed.

Watch for allergic reactions. Allergic reactions related to the radiotracer dye are rare, but they do happen and can be life-threatening. In most cases, the reaction is mild and causes some pain and inflammation at the injection site and a related skin rash. In severe cases, anaphylaxis is triggered and leads to a widespread allergic reaction causing swelling, breathing difficulty, hives, and reduced blood pressure. Call your doctor immediately if any signs of an allergic reaction become obvious once you get home after your appointment. The radioactive tracer takes between one to four hours to be absorbed by your bones, although most allergic reactions occur within 30 minutes of the injection.
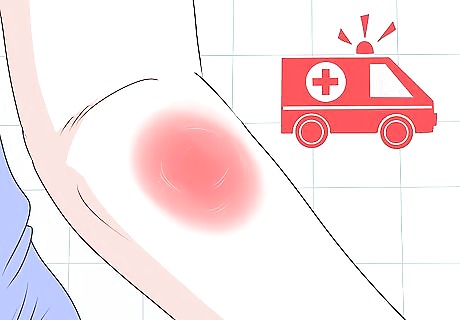
Look out for potential infection. There is a slight risk of infection or excessive bleeding when the needle is inserted into your vein to inject the radioactive dye. Infections usually take a couple of days to develop and include pain, redness, and swelling at the injection site. Call your doctor immediately if you notice these signs. You may need to go on antibiotics to combat the infection. Signs of a more significant infection include severe throbbing pain and pus drainage at the injection site, numbness and tingling in your involved arm, fatigue, and a fever. Make sure the doctor or technician cleans your arm with an alcohol swab or wipe just prior to the injection.
















Comments
0 comment