
views
Treating Esophageal Problems
See your doctor and take prescribed medications for infectious esophagitis. Esophagitis means your esophagus is inflamed. If you have esophagitis, you might feel a burning sensation in your chest (particularly after eating) or experience painful or difficult swallowing. Your doctor might perform an endoscopy and/or prescribe antibiotics, antivirals, or acid blockers. Your doctor may also request a blood test to find the root cause of the infection. If you have a weakened immune system, you’re more likely to get infectious esophagitis.
Heal esophageal ulcers with medication, dietary changes, or surgery. Esophageal ulcers are essentially sores that have formed on your esophageal lining after being exposed to lots of stomach acid. If you have GERD, you’re more likely to get ulcers. Your doctor might recommend proton pump inhibitors (like Prevacid or Prilosec—both available over-the-counter) or, if those don’t work, suggest fundoplication surgery. Fundoplication surgery is a common treatment for esophageal ulcers and the procedure is minimally invasive (meaning only small abdominal incisions are necessary). It involves tying a small bit of stomach muscle around the base of your esophagus to strengthen the esophageal sphincter. Changing your eating habits and avoiding GERD trigger foods (like spicy foods, mint, and chocolate) will help your esophagus heal along with medication. Barrett's esophagus is caused by acid reflux. The stomach acid comes up into the esophagus repeatedly and damages the lining. Patients have to take medication to decrease acid reflux and regular examinations by a gastroenterologist.

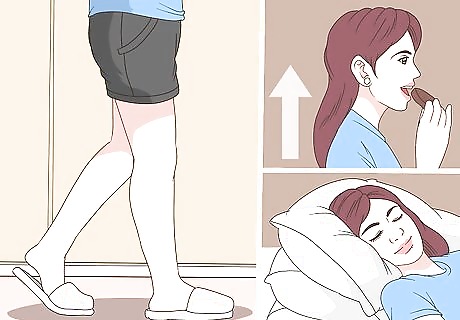
Take pills with a full glass of water to avoid esophageal irritation. Pills and capsules can sometimes get stuck in your throat, especially if you swallow them dry or with only a little bit of water. This means the pill can start dissolving in your throat, irritating the lining of your esophagus. Aspiring, antibiotics, quinidine, potassium chloride, vitamin C, and iron are especially known to irritate your esophagus if the pills or capsules get stuck. Take pills and capsules with a full 8 fluid ounces (240 mL) of water and take them while standing or sitting.
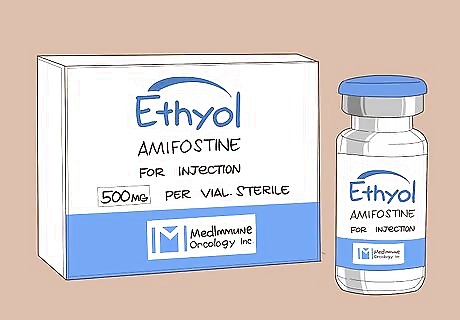
Ask your doctor about Ethyol to lower the risk of radiation esophagitis. Radiation esophagitis is a common adverse effect of cancer treatment. Luckily, amifostine (brand name Ethyol) can help lessen your risk when taken about 30 minutes before chemotherapy. You’ll need to ask your doctor for it ahead of time because it can only be administered intravenously. Make sure you’re eating nutritious foods and avoid anything super hot or spicy to help manage radiation esophagitis. Unfortunately, there’s no cure for this kind of esophagitis, but symptoms should start to go away about 2 to 4 weeks after your last chemotherapy treatment.

Visit your doctor for trouble swallowing or feeling something in your throat. While there are several causes for these symptoms, they can be a sign of a severe condition. To ensure you get the right treatment, see your doctor immediately for a proper diagnosis. Your doctor will figure out why you're having trouble swallowing or feel like you have something stuck in your throat so you can start treatment. If you don't get proper treatment, your condition could worsen. Play it safe and talk to your doctor.

Seek immediate treatment for bloody vomit or chest pain while vomiting. Try not to worry, but these symptoms may be a sign that you have a tear in the mucosa of your esophagus. Typically, this occurs when you cough or vomit a lot. If you see blood in your vomit or are feeling a lot of chest pain after you vomit, go to the emergency room or call for help so you can get the treatment you need. Typically, this condition needs to be treated in a hospital.
Adjusting Your Diet
Choose soft proteins with high moisture content. Soft, boneless fish fillets or tender ground meat with sauces or marinades are easier to swallow and won’t scratch your throat. Plus, the protein and amino acids will help heal your esophagus faster. Casseroles and stews are great options because the moisture will help the meats go down easier and ease digestion. Soft scrambled eggs are a great breakfast option. However, be wary of eggs if you think you might be allergic. Avoid fibrous or stringy meats that have bristle or peppercorn (like steak, spare ribs, sausage, and bacon).
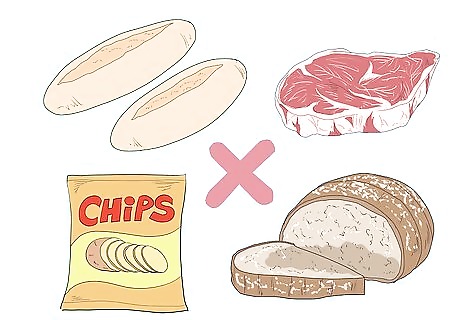
Avoid tough, chewy, and abrasive foods. If your esophagus is already inflamed, you want to avoid any foods that might scrape or scratch its fragile lining. Avoid chewy bread rolls, tough meats, hard bread crusts, and crispy chips. Cereal, granola, and seeded bread slices aren’t going to feel good going down, so choose well-cooked oatmeal instead (and make sure the oats have no added seeds or nuts). If you still want to eat bread, crackers, or chips, soften them up by putting them in soups or broths first.
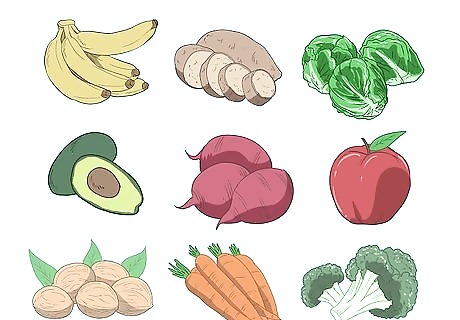
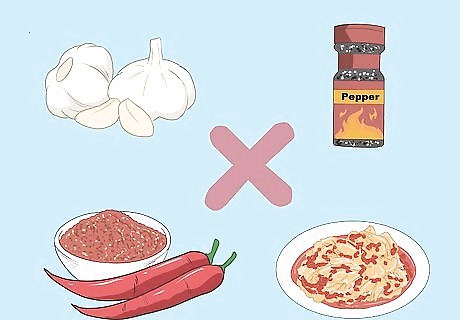
Cook vegetables thoroughly to soften them. Avoid eating raw vegetables (even lettuce for salads) and choose canned or well-cooked vegetables. Potatoes (without skins), squash, carrots, and spinach are all nutritious options that won’t irritate your throat. Cook vegetables with broth to add some flavor and help soften them up. Avoid fibrous vegetables like okra, artichokes, and celery. If you have GERD, alkaline veggies like asparagus, spinach, kale, and Brussels sprouts will help lower the amount of acid in your stomach. Avoid cooking your vegetables with onion or garlic as these are common triggers of acid reflux.
Opt for fruits and vegetables that are rich in soluble fiber. Fiber helps manage symptoms of acid reflux and GERD by speeding up gastric emptying and increasing pressure on the esophageal sphincter (which means stomach acid can’t easily travel up your esophagus). Root vegetables like potatoes, beets, carrots, and parsnips are a great source of fiber. Bananas are low in acid and contain pectin, a type of fiber that helps push food through your digestive system. This is helpful because food that stays in your stomach too long will create excess acid that might travel up your esophagus.
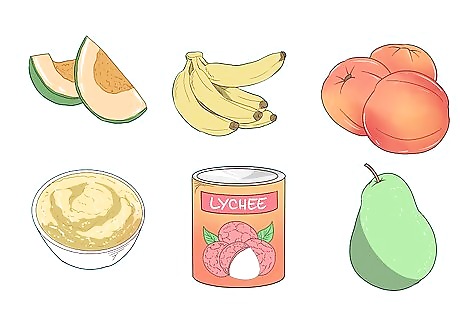
Eat soft canned, blended, or fresh fruits. Softer fruits like bananas, melons, and peaches are easier to swallow than hard and seeded fruits like apples and pomegranates. Canned pears, peaches, and lychee are all throat-friendly options that will provide some fiber and vitamin C for digestion and healing. Applesauce is delicious and easy to make at home! Avoid dried fruits because they’re too chewy (or crispy depending on the fruit) and might get stuck in your throat. You can still enjoy harder fruits if you juice them or blend them into a smoothie with milk or yogurt. Avoid citrus fruits (like oranges, tangelos, grapefruit, lemons, and limes) as they are highly acidic and might further any inflammation.

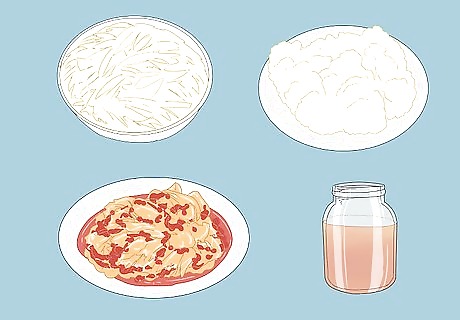
Incorporate probiotics for healthy gut flora and digestion. Adding more good bacteria to your gut biome increases how fast you digest food. As a result, the food and gastric juices in your stomach won’t sit around as long, making it less likely for acid reflux to occur. Enjoy sauerkraut, kefir, and yogurt to aid with digestion. Kimchi and kombucha also have probiotics, but their respective spiciness and carbonation can irritate the lining of your esophagus.
Indulge with soft, creamy desserts and snacks. Typical snack foods tend to be crispy or crunchy. Avoid popcorn, chips, and snacks containing nuts, seeds, or coconut flakes to avoid irritating your throat. Snack on applesauce, yogurt, or cottage cheese to satisfy your mid-afternoon cravings. End your meals on a sweet note with pudding or soft-baked cookies. You can even make your own (eggless) edible cookie dough to satisfy your sweet tooth.
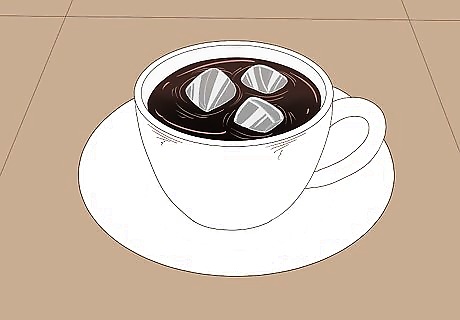
Avoid very hot or very cold liquids. Your esophagus is already sensitive, so while it may be tempting to sip on ice water, room-temperature water is a better option. Wait for coffee and teas to cool down a little and, if you must use ice, only use a few chunks. Carbonated drinks can also irritate the lining of your esophagus. If you have GERD, you should avoid both carbonated and caffeinated drinks. Switch to decaf!

Avoid spicy foods to decrease symptoms of esophagitis. Spicy foods irritate the lining of your esophagus and cause your stomach to produce more gastric acid. Excessive spice can also relax the muscular ring at the base of your esophagus, making it easier for acid to travel upwards. If you can’t give up spicy foods, chew on sugar-free (non-mint flavored) gum after a meal and go for a walk to help you digest.
Add ginger to your foods for an anti-inflammatory effect. Whether your esophagus is inflamed due to acid reflux, GERD, or other causes of esophagitis, ginger can help relieve that swelling. Ginger can also speed up gastric emptying (which means stomach acid has less of a chance to move upward). Sip on ginger tea or chew ginger gummies after eating. Slice raw ginger root very thin and add it to bowls, meats, soups, or smoothies. Ginger will also help relieve nausea related to chemotherapy.

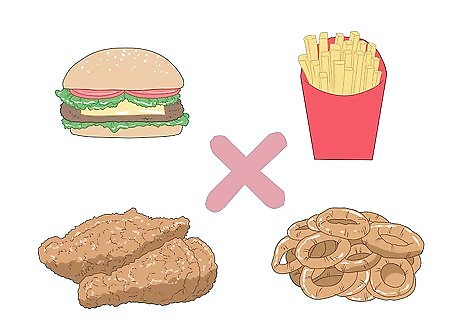
Avoid fried foods and foods containing trans fats. Fried foods are one of the worst things you can eat if you have esophagitis. Highly fatty foods (specifically trans fats) will cause your stomach to produce more acid, making it more likely for those gastric juices to irritation your esophagus. You can still eat fats, just stick to the good (monounsaturated) kinds. Eat healthy fats like avocado, olives, olive oil, flax seeds, chia seeds, nuts, and nut butters. However, some of these foods (particularly avocado and nuts) can trigger acid reflux if you’re allergic or have GERD. If this is the case for you, mayonnaise, sour cream, cream cheese, and light butter are other sources of fat that are considered less triggering for most people.
Making Lifestyle Changes

Avoid or limit your alcohol intake. Alcohol weakens the muscular ring connecting your esophagus to your stomach, allowing acid to seep upward. Alcohol also damages the mucus in your esophagus and your stomach, making it easier for acid to travel back up. If you do drink, avoid doing it 2 to 3 hours before bed. Stick to a maximum of 1 drink per day for women and 2 drinks for men and be sure to drink water before, during, and after consumption. One drink is equal to: 12 fluid ounces (350 mL) of beer (5% ABV) 8 fluid ounces (240 mL) of malt liquor (7% ABV) 5 fluid ounces (150 mL) of wine (12% ABV) 1.5 fluid ounces (44 mL) of distilled spirits or liquor (40% ABV)—like a shot of gin, rum, vodka, whiskey, or tequila
Quit smoking for your esophageal (and overall) health. Smoke dries out your esophagus and causes damage to your blood vessels. And, like alcohol, it relaxes the esophageal sphincter that acts as a gateway between your esophagus and stomach. Quit cold turkey or wean yourself off of tobacco by decreasing the amount of cigarettes you smoke each day. You can also use nicotine gum, lozenges, patches, sprays, and natural remedies to ease withdrawal symptoms. Chew on toothpicks or chew gum to satisfy oral cravings. Know your triggers (e.g., certain places you always smoke, friends who smoke, times of day that you routinely smoke) and avoid them or have a plan to manage your cravings.
Avoid eating right before bed. Your body produces more stomach acid as you digest, and when you lay down, it’s easier for the acid to work its way into your lower esophagus. While everyone digests at a different pace, wait about 2 to 3 hours before laying down after meals. Go for an easy 10- to 20-minute walk after meals to help speed up digestion and send gastric juices flowing as they should (down, not up!). Sit upright during and after meals. Prop your head and shoulders up with extra pillows when you sleep to create a slope that makes it harder for acid to travel upwards.

Chew non-minty gum to reduce the amount of acid in your esophagus. Gum makes you salivate, which neutralizes acid in your esophagus. Just be sure to choose gum that isn’t mint flavored (like peppermint or spearmint) because mint relaxes the flap at the base of your esophagus. Choose sugar-free gum—but note that artificial sweeteners (like sorbitol) can trigger acid reflux in some people. Chew gum about half an hour after eating to ease acid reflux.

Avoid caffeinated beverages. Unfortunately, caffeine is one of the most common acid reflux triggers for a lot of people. But don’t worry, you can still enjoy the taste of coffee by switching to decaf (which still has about 7 to 10 milligrams of caffeine). Swap black tea for herbal teas and avoid soda and energy drinks. If you’re a heavy coffee drinker (over 4 cups a day), wean yourself off of caffeine by drinking half-caffs before going strictly decaf.
Eliminating Trigger Foods for Eosinophilic Esophagitis

Eliminate milk, wheat, soy, eggs, nuts, and fish one by one for 6 weeks. Wheat and milk are the most common causes of EoE, so talk to your doctor about eliminating one of those for a week or two. If nothing changes, eliminate another food group as well. Check in with your doctor (this can be a primary care physician, nutritionist, allergist, or gastroenterologist) if or when you notice a change (like less pain during or after eating) while eliminating a certain food group. It may also be helpful to see an allergist for a skin-prick test to figure out your particular allergens. If you have EoE, you won't experience typical food allergy symptoms like tongue swelling, hives, and throat tightness. The symptoms of EoE are delayed and, over time, may cause narrowing of esophagus, scarring, and changes to your esophageal lining.
Ask your doctor about topical steroids to ease symptoms during the diet. While there are no medications specifically approved to treat EoE, topical steroids (like fluticasone or budesonide) can be used to manage inflammation and symptoms during an elimination diet. However, topical steroids should only be used for a short period of time and will probably only make a difference for mild EoE. Fluticasone and budesonide are typically used in asthma inhalers to prevent narrowing of the esophagus.
See your doctor after 6 weeks of an elimination diet. Your doctor will perform an esophagogastroduodenoscopy (EGD) at the 6 week mark along with a biopsy to check your esophagus for any inflammation, ulcers, or narrowing. If you have ulcers, they might prescribe medication and make dietary suggestions. Tell your doctor if you feel like your symptoms of EoE are getting better so you can start reintroducing foods again. They’ll probably give you the go-ahead if your EGD results show no signs of ulcers or severe inflammation that requires more intense treatment. Always read food labels to check for certain allergens. Work with a nutritionist to make sure you’re getting all of your daily nutrients while on an elimination diet.
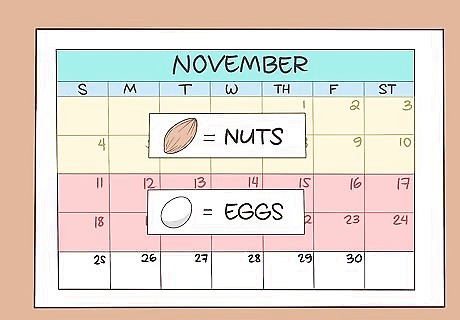
Reintroduce foods one at a time for 2 weeks each. If your EGD results show improvement in the lining of your esophagus, work with your doctor to reintroduce the eliminated foods one at a time. Allow 2 weeks for each reintroduced food group and see or contact your doctor at the end of each 2 week trial. For example, reintroduce nuts for 2 weeks and if no reaction occurs, start including eggs for two weeks and so on. If you feel your throat narrowing or if swallowing becomes difficult, stop eating the food, tell your doctor, and don’t introduce anything new for about a week or two so your esophagus can recover. If you have a skin prick test and discover that you are allergic to any of these trigger foods, don’t reintroduce them into your diet. If the condition of your esophagus worsens, your doctor might suggest surgery.



















Comments
0 comment