views
X
Trustworthy Source
National Heart, Lung, and Blood Institute
Research and education center within the National Institutes of Health
Go to source
In many cases, managing angina pain can be done with home remedies and with changes to your diet and lifestyle.
Diagnosing Angina Pain

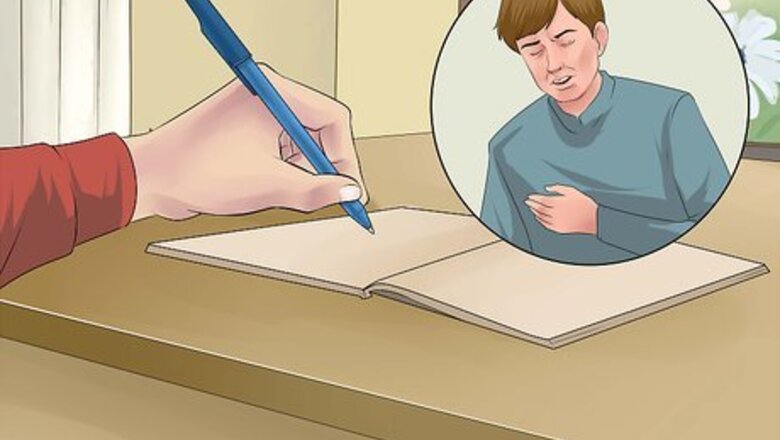
Keep a journal. Write in a journal to track patterns or changes in your daily routine. This can help your doctor determine if your pain is a result of an underlying heart problem, especially if you experience chest pain frequently. Angina can be a sign of coronary heart disease (CHD), even if initial tests don't point to the disease. However, not all chest pain or discomfort is a sign of CHD. Panic attacks and other lung or heart conditions can also cause chest pain. Your doctor may ask about your symptoms, risk factors for heart disease, and your family history regarding CHD and other heart conditions. Take note of the following things in your journal: What the pain feels like, symptoms you experience when you have chest pain, such as high blood pressure, and any symptoms you experience afterwards, such as nausea or dizziness. How often you experience chest pain, where you feel pain or discomfort, the severity of the pain and how long the pain lasts. Dietary changes or foods you ate two to three days prior to experiencing chest pain or indigestion. Also note any beverages such as coffee, tea, and soda, and how frequently you drink them per day or per week. New exercise regimes or recreational activities that cause physical exertion. Any stressful environments, work or relationships that may be causing symptoms of chest pain. Any other conditions you may have or any illnesses you may have had, such as a fever or cold, prior to experiencing chest pain. Any drugs, medications, supplements, herbs or home remedies you are currently using or may have used in the past two weeks. If your chest pain is interfering with your daily activities.
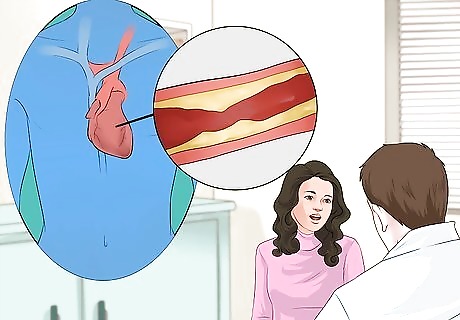
Visit your doctor for diagnosis. Any kind of chest pain should be checked by your doctor, since it may be a symptom of an underlying condition. Your doctor may suggest lifestyle changes, medicines or medical procedures depending on the type and severity of your angina pain. Different types of angina have different symptoms and require different treatments. If you have angina, you may diagnosed with one of the following: Stable angina: Stable angina is the most common type which follows a regular pattern, such as when it occurs and what factors may trigger it. It usually occurs after stress or physical activity and may last one to 15 minutes. Stable angina isn’t a heart attack, but suggests that a heart attack is more likely to occur in the future. If you have stable angina, you can learn its pattern and predict when the pain will occur. The pain usually goes away a few minutes after you rest or take your angina medicine (usually nitroglycerin, taken sublingually or under the tongue). Variant angina: Variant angina is rare. A spasm in a coronary artery causes this type of angina. Variant angina usually occurs while you're at rest, and the pain can be severe. It usually happens between midnight and early morning. Smoking is a major risk factor for this type of angina. Medicine can relieve this type of angina. Unstable angina: Unstable angina doesn’t follow a pattern and it may occur more often and be more severe than stable angina. It often occurs while the person is at rest. This type is very dangerous as it suggests that a heart attack may happen soon and requires emergency treatment. Unstable angina also can occur with or without physical exertion — it often happens without physical activity. Rest or medicine may not relieve the pain. Microvascular angina: Microvascular angina can be more severe and last longer than other types of angina. It is often noticed during routine activities and times of psychological stress. Symptoms include shortness of breath, sleep problems, fatigue and lack of energy. Medicine may not relieve this type of angina.
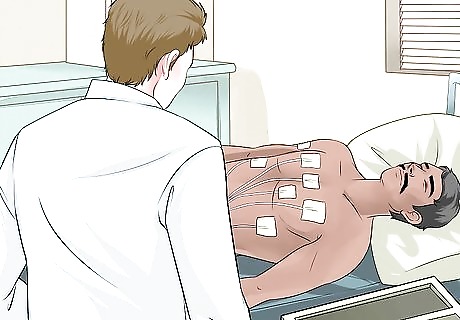
Consider an electrocardiogram. Your doctor may suggest getting an electrocardiogram (ECG) to determine if you may have heart disease. If you experience angina pain or palpitations, an electrocardiogram is usually the first test to determine if you have heart disease. An ECG is a test that records the electrical activity of the heart to measure any damage to the heart, heart rate, size and position of heart chambers. It also measures the effects of drugs or devices you may be using to manage chest pain. In addition, an ECG can be used to monitor stress levels. The procedure for ECG is painless, done by attaching patches called electrodes to your arms, legs or chest to monitor heart activity. Ask your doctor about an ECG if you experience angina pain and have had heart problems in the past or have a strong history of heart disease in your family. Make sure your healthcare provider knows about all the medications you are taking, as some can interfere with test results. Exercising or drinking cold water immediately before an ECG may cause false results.
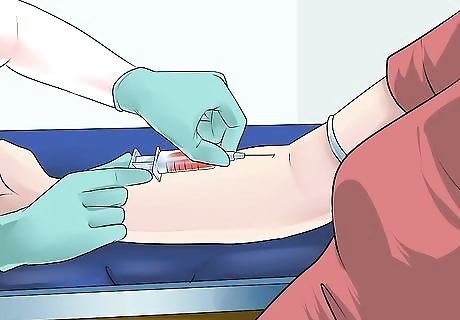
Get a blood test. Blood tests check the levels of certain fats, cholesterol, sugar, and proteins in your blood. Abnormal levels may show that you have risk factors for coronary heart disease. Your doctor may recommend a blood test to check the level of a protein called C-reactive protein (CRP) in your blood. High levels of CRP in the blood may increase the risk for coronary heart disease and heart attack. Your doctor also may recommend a blood test to check for low levels of hemoglobin in your blood. Hemoglobin is an iron-rich protein in red blood cells. It helps the blood cells carry oxygen from the lungs to all parts of your body. If your hemoglobin level is low, you may have a condition called anemia.
Improving Your Lifestyle

Drink lots of water. Water helps flush out excess sodium that causes high blood pressure and hypertension. These symptoms often lead to angina pain and coronary heart disease. Aim to drink at least eight ounces of water every two hours. 2 liters of water is the daily recommendation for the average adult. If you take caffeinated beverages, take 1 liter of water for every cup (1 fluid oz.) of caffeine. If you are taking blood-thinning medications or diuretics (water pills) for angina pain, ask your doctor about how much water you should consume. Not getting enough water can also lead to dehydration. Dehydration can cause headaches, irritability, dizziness, irregular heartbeat and shortness of breath. Non-caffeinated, glucose-free sports drinks with electrolytes can help alleviate dehydration as well.

Get enough sleep. Not getting enough sleep has been linked to increased risk of high blood pressure, hypertension, diabetes, obesity and chronic stress, all of which can cause angina pain and increase the risk for heart disease. Studies show that sleep deprivation can weaken the immune system, increase the production of stress hormones, put you at higher risk for chronic disease and lower life expectancy. If you suffer from sleep apnea or insomnia, talk to your doctor for possible treatments. Other ways you can make sure you get enough sleep include: Avoid caffeine, nicotine, alcohol and sugary drinks four to six hours before sleeping. These can act as a stimulant to keep you awake. A quiet, dark, and cool environment can help promote sleep. Use heavy curtains or an eye mask to block light. Light is a powerful cue that tells the brain that it's time to wake up. Keep the temperature comfortably cool (between 65 and 75°F or 18.3 to 23.9°C), and keep the room well ventilated. Make sure your bedroom is equipped with a comfortable mattress and pillows. Change your sheets and pillow covers often. If you have trouble breathing, try to prop your head up on a pillow to improve air flow. Struggling to fall asleep just leads to frustration. If you’re not asleep after 20 minutes, get out of bed, go to another room and do something relaxing until you are tired enough to sleep. Avoid activities such as work or exercise three to four hours prior to sleeping. Physically and psychologically stressful activities can cause the body to secrete the stress hormone cortisol, which is associated with increasing alertness. Try listening to relaxing music or doing some light reading a few hours before sleeping. Having a regular sleep schedule helps to ensure better quality and consistent sleep. Try to set a routine by going to bed early and waking up early to set your body’s internal clock. If you have congestive heart failure in addition to angina you may need to elevate the bed with pillows when you sleep so that your head is above your heart.

Avoid sitting for long periods. Sitting idly greatly increases the risk for angina pain and other heart diseases. Do not sit in front of the TV, behind a work desk or driver’s seat for more than two hours if you have been diagnosed with angina. Think about ways you can walk while you work, such as standing while talking on the phone. Take five minute breaks between work to stretch your arms and legs. The muscle activity needed for standing and other movement seems to trigger important processes related to the breakdown of fats and sugars within the body. When you sit, these processes stall and your health risks increase. When you're standing or actively moving, you kick the processes back into action.

Avoid stress. While a small amount of stress is healthy, it can cause blood pressure, anxiety, irregular heartbeat and alter immune function, triggering angina pain and in severe cases cause heart attacks. As people age, achieving a relaxation response after a stressful event becomes more difficult. To avoid stress, practice meditation exercises like yoga and tai chi, make time for recreation and be sure to get enough rest. Other simpler ways to reduce stress are: Slow, deep breathing in a quiet environment. Breath in through your nose and out through your mouth. Try and feel the diaphragm muscle when you breath in order to stimulate the parasympathetic nervous system. Focus on positive outcomes. Restructure priorities and eliminate unnecessary tasks. Reduce use of electronic devices. These may cause eye-strain and trigger headaches. Use humor. Research has found humor to be an effective way to deal with acute stress. Listen to relaxing music.

Get moderate exercise. Studies show that regular exercise is beneficial for individuals with stable angina as it helps regulate high blood pressure, cholesterol, diabetes and obesity. Aerobic exercise, in particular, increases blood and oxygen flow to the heart while at rest and when you're doing everyday things like climbing stairs or carrying groceries. It also helps reduce the body’s production of stress hormones and has a positive impact on psychological health., Talk with your healthcare practitioner or a registered clinical exercise physiologist (RCEP) before starting an exercise program. Ask for specific program recommendations to improve cardiovascular fitness, increase muscle strength and endurance, and improve range of motion. An extended warm-up and cool-down may reduce the risk of angina or other cardiovascular complications following exercise. Warming up and cooling down are important parts of every exercise routine. They help the body make the transition from rest to activity and back again, and can help prevent soreness or injury, especially in older people. Choose low-impact activities such as walking, cycling or water exercises, which involve large muscles groups and can be done continuously. If your fitness level is low, start with shorter sessions (10 to 15 minutes) and gradually build up to 30 minutes five or more days per week. Perform light-resistance circuit training and whole-body range-of-motion exercises two to three days per week. Closely monitor your intensity level and stay within your recommended target heart-rate zone. Take frequent breaks during activity if needed. Stop exercising immediately if you experience angina. Contact your physician if you experience chest pain, labored breathing or extreme fatigue. Don’t eat for two hours prior to exercise. Drink plenty of fluids before, during and after a workout. If nitroglycerin has been prescribed, always carry it with you, especially during exercise.
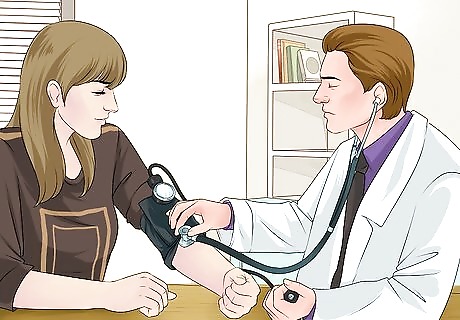
Monitor your blood pressure. Irregular heartbeat, high or low blood pressure and increased stress can trigger angina pain, and in severe cases cause heart attack. Your doctor may ask you to keep track of your blood pressure at home. To do this, you will need to get a home blood pressure monitor. The monitor you choose should be of good quality and fit well., Digital monitors are the best choice for most people. Practice using the monitor with your doctor or nurse to make sure you are taking your blood pressure correctly. A digital blood pressure monitor will not be as accurate if your body is moving when you are using it. Also, an irregular heart rate will make the reading less accurate. Your arm should be supported, with your upper arm at heart level and feet on the floor with your back supported and legs uncrossed. It's best to measure your blood pressure after you rest for at least five minutes. Blood pressure should not be checked right after experiencing stress, exercise, tobacco exposure, or consuming foods or beverages, such as coffee, that can raise blood pressure. If your blood pressure monitor shows a reading of more than 120/80 mmHg, you may have moderate hypertension. If it shows a reading higher than 140/90 mmHg, you may have high blood pressure and should tell your doctor. All adults should have their blood pressure checked every one to two years if their blood pressure was less than 120/80 mmHg at their most recent reading.

Apply a warm towel compress. Soak a small towel in lukewarm water (104–113°F or 40–45ºC), then wring the water out. Lie down and apply the warmed towel to your chest or mid-back for 20 to 25 minutes. This helps improve circulation in the arteries and reduce spasms to relieve acute anginal pain within five to 10 minutes. If the pain is extremely severe, causes dizziness or shortness of breath, you should seek medical care immediately.

Take warm showers. Taking lukewarm showers (104–113°F or 40–45ºC) for five to 10 minutes can help improve circulation and reduce muscle pain, thus decreasing the chance of angina pain. You can do this up to two or three times per week. Taking frequent showers or showers longer than 15 minutes is not recommended as it can cause dry skin.

Quit smoking. Smoking, secondhand smoke, exposure to carbon monoxide and taking in any form of nicotine can aggravate symptoms of angina pain. It can also cause hypertension and an irregular heartbeat, and it can constrict blood vessels. This increases the risk of having a heart attack and frequent angina pain. Try to avoid exposure to smoke and hazardous fumes in your environment. If you currently smoke, ask your doctor about ways to quit smoking.

Limit alcohol intake. A moderate amount of alcohol, whether it is wine, beer or spirits, can help lower the risk of heart disease and heart-related conditions such as angina. However, alcohol should be taken in moderation. If you have a condition related to angina, such as high blood pressure, high cholesterol, arrhythmia (irregular heartbeat) or diabetes, you should reduce alcohol intake to one drink a day for women, and two per day for men. , Avoid alcoholic drinks if you are: someone recovering from alcohol addiction, pregnant or breastfeeding women, someone with a family history of alcoholism, someone with liver disease, or someone taking one or more medications that interact with alcohol.
Eating a Healthy Diet

Avoid inflammatory foods. Foods that cause inflammation can increase your risk for heart disease, diabetes, high blood pressure and high cholesterol. They can also cause indigestion, bloating, stress and depression, all of which can trigger angina pain. These foods are also high in saturated fats, which can cause blood clotting, constricted blood vessels and plaque formation in the heart’s arteries, increasing the risk of heart attack in people with angina. Try to avoid these foods as much as possible: Refined carbohydrates such as white bread, pastries and donuts Fried foods Sugar-sweetened beverages such as soda or energy drinks Red meat such as veal, ham or steak and processed meats such as hot dogs Margarine, shortening and lard
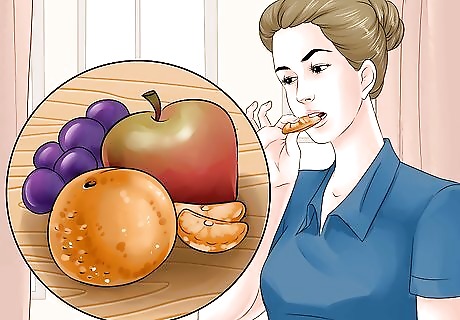
Eat certain fruits to improve heart health. Certain fruits can be effective in stopping angina pain. Because they are rich in antioxidants, they aid in purifying and thinning the blood, eliminating toxins and improving blood circulation. They are also a rich source of essential minerals, vitamins and nutrients. They may help to improve your immunity and the elasticity of your blood vessels. Fruits that promote heart health, and thereby reduce angina pain, include: Grapes Pineapples Strawberries, blueberries and cherries Oranges Pomegranates Apples

Eat vegetables that may help to reduce angina pain. Vegetables that are rich sources of minerals, vitamins and nutrients may aid in managing cholesterol, reducing inflammation and regulating blood flow to reduce risk of angina pain and other heart diseases. Some vegetables to include in your diet include: Leafy vegetables such as spinach, kale, collard greens, lettuce and cabbage Broccoli Green beans Sprouts Carrots Tomatoes
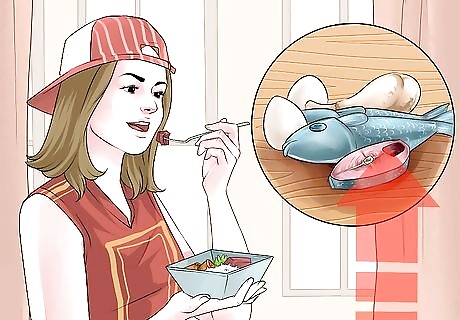
Increase your intake of foods with essential fatty acids. Eggs, fish and lean poultry meats contain essential omega-3 and omega-6 fatty acids. These acids help lower bad cholesterol that can cause obesity and plaque formation in the arteries. They also help reduce stress and improve blood circulation and immune function. These factors will help reduce the risk of heart disease, heart attack and angina pain.,, Foods that are high in omega-3 fatty acids are are: Eggs Flaxseed Fatty fish such as salmon, tuna, mackerel and shrimp Poultry meats such as quail, turkey and chicken Nuts such as walnuts, almonds, and Brazil nuts

Use heart-healthy cooking oil. Some vegetable oils such as flaxseed, canola, olive, and soybean are rich in omega-3 and omega-6 essential fatty acids, which help reduce cholesterol and reduce the risk of heart disease. Replacing your regular vegetable cooking oil with a healthier alternative can help decrease the risk of angina pain., , You can also use these oils for salad dressings.

Add honey to your diet. The phenolic constituents in honey such as quercetin, acacetin and galangin may help to treat cardiovascular conditions. Flavonoids in honey may also decrease your risk of other heart conditions. Because of this, honey may improve blood circulation, oxygen supply in the blood, and may enhance the functioning of your organs. It can also reduce the accumulation of fat in your arteries, thereby reducing the possibility of angina pain. Eat a teaspoon of wild honey in the morning every day. You can also add ½ teaspoon of honey to decaffeinated tea or glass of water and drink the mixture, up to three times per day. Make sure the honey does not contain added sugars, as these sugars can increase the risk of diabetes when used for a long period.
Taking Heart-Healthy Supplements
Get more Vitamin C. Vitamin C is an important natural antioxidant that helps promote immune function, manage blood sugar, and stimulate cell growth and repair. Vitamin C also lowers the risk of various chronic diseases including angina pain and coronary heart disease. Although vitamin C deficiency is rare, it can greatly affect the immune system. Vitamin C can be taken as a dietary supplement with a recommended dose of 500 mg split into two or three times daily. You can also add vitamin C-rich foods to your daily diet. Good natural sources of vitamin C are: Sweet red or green peppers Citrus fruit such as oranges, pomelo, grapefruit, limes or non-concentrated citrus juices Spinach, broccoli and Brussel sprouts Strawberries and raspberries Tomatoes Mango, papaya and cantaloupe Since smoking depletes vitamin C, smokers may need an additional 35 mg per day.

Increase your intake of niacin. Niacin is a form of vitamin B3 used to improve blood flow and lower bad cholesterol levels. High cholesterol causes plaque to build up in your arteries. Lowering your cholesterol reduces the risk for angina and heart disease. Niacin may also help regulate blood sugar levels for type 1 and type 2 diabetes. The recommended dosage for niacin are 14 to 18 mg per day, whether taken as a supplement or through a food source. Do not take a higher dosage unless recommended by your doctor. People with coronary artery disease, severe or unstable angina should not take niacin without their doctor’s supervision. Large doses can raise the risk of heart rhythm problems. The best food sources of vitamin B3 are found in beets, brewer's yeast, beef liver, beef kidney, fish, salmon, swordfish, tuna, sunflower seeds, and peanuts. Bread and cereals are usually fortified with niacin. In addition, foods that contain tryptophan, an amino acid the body converts into niacin, include poultry, red meat, eggs, and dairy products. Niacin is available as a tablet or capsule in both regular and timed-release forms. The timed-release tablets and capsules may have fewer side effects than regular niacin. However, the timed-release versions are more likely to cause liver damage. Doctors recommend periodic liver function tests when using high doses (above 100 mg per day) of niacin.
Get enough magnesium. Magnesium is a necessary nutrient for many body functions, contributes to energy production. It regulates anxiety, stress, chronic fatigue, and helps maintain healthy blood pressure, cholesterol and blood sugar levels to reduce the risk of angina and other heart diseases. Magnesium deficiency can also weaken the immune system and cause a number of health problems. Natural food sources of magnesium are salmon, mackerel, halibut, tuna, dark chocolate, dark leafy greens, nuts, seeds, brown rice, lentils, soybeans, black beans, chickpeas, avocado, and bananas. Calcium can inhibit the absorption of magnesium supplements, so it is better to use more readily absorbed forms such as magnesium bicarbonate and magnesium oxide. 100 mg of magnesium supplements is recommended to be taken two to three times daily. Adults should get at least 280–350 mg of magnesium daily. Symptoms of magnesium deficiency may include agitation and anxiety, restless leg syndrome (RLS), sleep disorders, irritability, nausea and vomiting, abnormal heart rhythms, low blood pressure, confusion, muscle spasm and weakness, hyperventilation, insomnia, and even seizures. Excessive intake of magnesium can have adverse effects and reduce calcium absorption, so it is important not to overdose. Ask your doctor what dosage will be right for your individual needs.

Take resveratrol. Resveratrol is an active compound found in grapes, grape seed and berries. It is shown to have beneficial effects on cardiovascular health by reducing high cholesterol, high blood pressure, diabetes and plaque formation in arteries, thereby managing and preventing angina pain. Resveratrol is available as a liquid extract, capsules or tablets at most pharmacies and nutrition stores. The recommended dosage for resveratrol is 30 to 45 mg after meals, up to three times per day.
Using Herbal Remedies
Drink lemon water. Some studies show that lemon juice contains antioxidants that can help with weight loss, manage high cholesterol levels and flush out excess sodium in the bloodstream. This will help reduce plaque build-up in the arteries and avert angina pain. Squeeze half a lemon into a cup of warm water and drink this mixture on an empty stomach in the morning. You may also add lemon juice as flavoring to your regular foods.

Increase your intake of garlic. Garlic is used for many conditions related to the heart and circulatory system, such as hypertension, irregular heartbeat, high cholesterol, coronary heart disease, heart attack, and to reduce plaque build-up in the arteries, thereby managing angina. This is because garlic contains a component called allicin, which aids in relaxing hard blood vessels. Garlic can also help reduce headaches, stress and promote healthy liver function. Eat one clove of raw garlic in the morning. If you do not like eating raw garlic, you can add minced or chopped garlic as a flavoring to your meals. Garlic supplements are also available at most pharmacies and nutrition stores. The recommended dosage for aged garlic extract is 600 to 1200 mg daily, divided into two to three doses. Garlic capsules or tablets should contain 0.5–1.5% of alliin or allicin to be beneficial, at a dosage of two 200 mg tablets, three times a day. People using prescription or blood-thinning medications, or those with ulcers and thyroid problems, should ask their doctor before using garlic or garlic supplements.

Eat ginger. Gingerol, a natural compound in ginger root, may help to lower blood cholesterol levels thereby potentially helping to prevent angina pain from occurring. It is also an antioxidant that protects the blood vessels from damage by cholesterol, helps manage stress and lower blood pressure., Do not take more than 4 gram of ginger per day without asking your doctor. Ginger should not be used with blood-thinning, hypertension or diabetic medications. Ginger can be added to your diet in many ways. You can boil 2–4 grams of ginger in a 1 cup of water to make unsweetened ginger tea. You can also take a ginger supplement, which are available at most pharmacies or add chopped ginger to your food.

Take ginseng supplements. Studies show that ginseng contains antioxidants that can help fight off free radicals, and improve heart health by regulating blood pressure, high cholesterol, blood sugar levels, reduce stress and improve physical strength and endurance, thus reducing the risk for angina and heart disease. Ginseng comes in different forms, such as liquid extracts, powders and capsules, and is often used in combination with other herbs or nutrients. Ask your doctor before using ginseng, especially if you are using prescription medications to manage angina. Your doctor will help determine the right dosage for you.

Try turmeric powder. Curcumin, the active compound in turmeric, inhibits plaque formation in your arteries and reduces bad cholesterol levels, both of which can lead to angina pain. Turmeric may also aid in managing obesity that can lead to other heart conditions, as well as reducing arthritis pain. Turmeric and curcumin supplements are considered safe when taken at the recommended doses. The recommended dosage for adults is 400–600 mg, up to three times per day. Taking large amounts of turmeric for long periods of time may cause stomach upset and, in extreme cases, ulcers. People who have gallstones or obstruction of the bile passages should talk to their doctor before taking turmeric. Add 1 teaspoon of turmeric powder to a cup of warm milk to create a heart-healthy drink that can be taken one to three times per day. You can also add a pinch of turmeric powder to your cooking for flavor. Ask your doctor before using turmeric if you are taking blood-thinning or diabetes medications.
Seeking Medical Care

Watch for severe symptoms. See your doctor right away if you have new, unexplained chest pain or pressure. You should call 911 if your chest pain does not go away five minutes after taking medication, increases in severity or if a person with angina loses consciousness. Other situations in which you should call your doctor are: You experience new or recurrent angina symptoms more often. You experience angina pain while sitting or resting. You have trouble taking your heart medication You feel tired, faint or lightheaded more often. You experience an irregular heartbeat, low (below 60 beats per minute) or high (above 120 beats per minute) blood pressure. You experience any other unusual symptoms that may be related to angina.
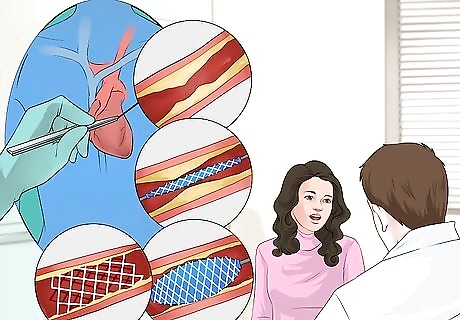
Ask your doctor about angioplasty. Angioplasty is a non-surgical, minimally invasive procedure used to open blocked or narrowed arteries, improving blood flow to the heart. Angioplasty can be performed by a licensed cardiologist to help treat moderate to severe angina pain caused by plaque build-up in the arteries. During an angioplasty, a small balloon is expanded inside the coronary artery to help compress the blockage and expand the artery wall. A wire mesh tube called a stent is sometimes implanted to keep the artery wall expanded. The procedure can last for two to three hours. Ask your doctor if an angioplasty may help your condition.

Consider EECP therapy. Enhanced external counterpulsation (EECP) therapy is a non-invasive procedure helpful for some people who have persistent angina. Large cuffs, similar to blood pressure cuffs, are put on your legs. The cuffs are inflated and deflated in sync with your heartbeat. EECP therapy improves the flow of oxygen-rich blood to your heart muscle and helps relieve angina. You typically receive 35 one-hour treatments over a period of seven weeks. EECP therapy can be performed by a licensed therapist or physician.
Ask your doctor about medication. Talk with your doctor if you have any questions or concerns about taking your angina medicines. You should know what medicines you're taking, the purpose of each, how and when to take them, possible side effects and if they are safe to take with other medicines, herbs or foods. If you have side effects from your medication, let your doctor know. You should never stop taking your medication without your doctor's approval. Your doctor may prescribe medicine to treat CHD, high blood pressure, diabetes, or high cholesterol levels. These may include: Anti-platelet drugs, also called blood-thinners, such as aspirin. Take the baby strength (81 mg) aspirin or cut the regular strength (325mg) aspirin in half. Take one pill once a day with food. Studies have shown that taking aspirin decreases your risk of a cardiovascular disease. ACE inhibitors to treat hypertension and high blood pressure Beta-blockers to treat hypertension, irregular heartbeat, angina pain and to prevent a heart attack. Calcium channel blockers for angina pain and hypertension Diuretics (water pills) to flush out excess sodium Statins to lower cholesterol Nitroglycerin pills or nitrates to stop an angina attack

Make an emergency action plan. Angina increases your risk for a heart attack. It’s important that you and your family know how and when to seek medical attention. Talk with your doctor about making an emergency action plan. Discuss your emergency plan with your family members. Take action quickly if your chest pain becomes severe, lasts longer than a few minutes, or isn't relieved by rest or medicine. The plan should include making sure you and your family members know: The signs and symptoms of a heart attack How to use medications when needed, such as nitroglycerin How to access emergency medical services in your community The location of the nearest hospital that offers 24-hour emergency heart care. Call 911 if you experience unstable angina, a heart attack, or loss of consciousness. You should also call 911 if the pain lasts longer than usual or if the pain returns a few minutes after taking medication.

Take nitroglycerin for immediate relief. Nitroglycerin is used to prevent chronic or stable angina. This medicine works by relaxing the blood vessels and increasing the supply of blood and oxygen to the heart. This medicine is also used to relieve an angina attack that is already occurring. When used regularly on a long-term basis, or just before exercise or a stressful event, this helps prevent angina attacks from occurring. Your doctor may prescribe nitroglycerin as a tablet, capsule or spray to help relieve angina pain. This medicine should be used exactly as directed by your doctor. Do not take more than the prescribed dose, do not take it more frequently, and do not take it for a longer time than your doctor ordered. If you miss a dose of this medicine, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not take double doses. When you begin to feel an attack of angina starting such as chest pains, tightness or squeezing in the chest, sit down. Use a nitroglycerin tablet or spray as directed by your doctor. You may become dizzy, lightheaded, or faint soon after using a tablet or spray, so it is safer to sit rather than stand while the medicine is working. If you become dizzy or faint while sitting, take several deep breaths and bend forward with your head between your knees. Remain calm and you should feel better in a few minutes. Nitroglycerin sublingual tablets usually give relief in one to five minutes. Nitroglycerin sublingual tablets should not be chewed, crushed, or swallowed. They work much faster when absorbed through the lining of the mouth. Place the tablet under the tongue or between the cheek and gum, and let it dissolve. Do not eat, drink, smoke, or use chewing tobacco while a tablet is dissolving. If the pain is not relieved, you may use a second tablet five minutes after you take the first tablet. If the pain continues for another five minutes, a third tablet may be used. Ask your doctor or nurse how to properly use a nitroglycerin oral spray if prescribed. You may administer one or two sprays of nitroglycerin oral spray at the onset of chest pain. If the pain continues after five minutes, a third spray may be used. You must wait five minutes after the first one or two sprays before using a third spray. If you still have chest pain after a total of three tablets or three sprays, contact your doctor or go to a hospital emergency room right away. Do not drive yourself and call 911 if necessary. Tell your doctor if you have any other respiratory or heart conditions. Also alert your doctor if you are using any other medications, supplements, herbal or home remedies, or if you experience an allergic reaction to nitroglycerin. Nitroglycerin should not be used for severe or unstable angina, during a heart attack, to treat low blood pressure or for people with anemia. Call 911 if you or someone with angina experiences a heart attack. Consult your doctor and see if nitroglycerin interacts with any of you current medication.



















Comments
0 comment