
views
Adjusting Your Sleeping Position

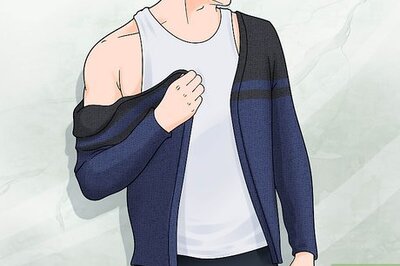
Sleep on your back with your head elevated if possible. Keeping your upper body elevated puts gravity to work for you, potentially making it more difficult for stomach acid to reach and irritate your ulcer. Additionally, sleeping on your back reduces the compression of your digestive system, which can also reduce ulcer pain. Unfortunately, depending on the location of your stomach ulcer, sleeping in this position may not necessarily cause a great deal of relief. But it’s definitely worth a try! Elevate your head with a wedge pillow, or use wood blocks to raise the head of your bed. If you find this sleeping position so uncomfortable that it makes it hard for you to sleep, you may be doing more harm than good. Try sleeping on your side instead. Putting a pillow under your knees can help take the pressure off of your stomach.
Lay on your left side if you’re a side-sleeper. If sleeping on your back doesn’t suit you, opt for sleeping on your left side instead of your right. Because of the layout of your digestive system, staying on your left side may cause less compression and less ulcer pain. As with sleeping on your back, this isn’t a guaranteed solution, depending on the location of your stomach ulcer. Placing a pillow between your knees may make side-sleeping more comfortable.

Don’t compress your digestive system by sleeping on your stomach. This is typically the worst sleeping position for a stomach ulcer or other stomach acid-related troubles (such as GERD). If you’re naturally a stomach-sleeper, try your best to get used to sleeping either on your back or your left side instead. Sleeping on your stomach is also harder on your back and neck than other sleeping positions.
Creating a Good Sleep Environment

Cut out caffeine, big meals, and screen time in the evening. Start planning for bedtime several hours before you actually go to bed! Avoid caffeine at or after dinner, and possibly anytime after lunch. Don’t eat any meals or large snacks within 3 hours of your bedtime. And steer clear of screens like TVs, computers, smartphones, and tablets for at least an hour before bed. The stimulant effect of caffeine counteracts your body’s preparation for sleep. Eating before bedtime puts your digestive system to work instead of letting it rest, makes you feel bloated and uncomfortable, and causes excess stomach acid production. The “blue light” produced by electronics screens may interfere with your body’s natural circadian rhythm that dictates your sleep cycle. If you can, use dimmable lights and reduce their intensity as you get later into the night This can help increase melatonin so you get better, healthier sleep.
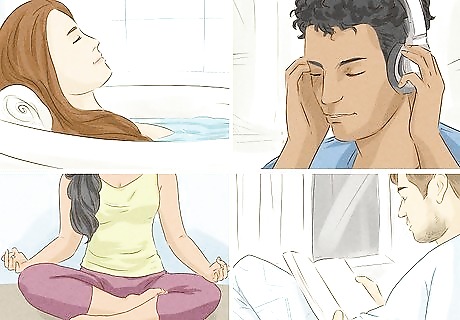
Create a consistent bedtime routine so you’re ready to sleep. By sticking to a steady routine each night, you can essentially train your body to be ready for sleep. For about 1 hour before going to sleep, complete a series of relaxing, calming activities that signal sleepy-time! For instance, you may try: Taking a warm bath with Epsom salt and up to 20 drops of lavender essential oil. Massaging your feet, legs, arms, and neck, especially while you’re in the tub. Laying out your clothes for tomorrow while listening to soothing music. Meditating or praying. Listening to relaxing music Reading a few pages of a calming book.

Make your sleeping area cool, quiet, dark, and comfortable. The more snooze-friendly your sleeping area is, the more likely you’ll be to fall asleep and stay asleep despite your discomfort. Try measures like the following: Keep the room as dark as you can. Use blackout curtains and remove light sources such as night lights and bright clock displays from the room. Set the thermostat on the cool side of room temperature, perhaps around 65–68 °F (18–20 °C). Shut doors or windows, if possible, to block sources of ambient noise, such as street traffic. Alternatively, use a white noise machine to mask unwanted sounds. Sleep on a good mattress with soft, comfortable bedding and a supportive pillow. Use an air purifier with a HEPA filter to help improve the air quality in your room. It can also make a soothing humming noise that may cancel out other noises and help you fall asleep.

Treat sleep apnea and other sleep disorders with your doctor’s help. It’s a vicious cycle—stomach ulcers make it harder to sleep, and not getting enough sleep can make gastrointestinal illnesses like stomach ulcers more likely. Since the problems are connected, treat them both at the same time. Along with getting medical treatment for your stomach ulcer, talk to your doctor about diagnostic and treatment options for any sleep disorders you may have. Sleep apnea can be a life-threatening condition if left untreated. It also makes you more likely to develop stomach ulcers.
Treating Your Ulcer Symptoms
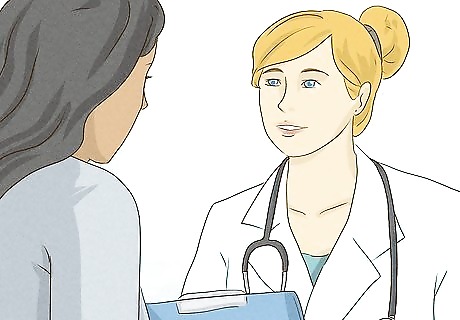
Get a clear diagnosis and treatment plan from your medical provider. Don’t just assume you have a stomach ulcer, and definitely don’t just wait for it to go away! Instead, visit with your doctor and undergo any tests required for them to reach a diagnosis. Then, discuss which treatment options are appropriate for your condition. The most common symptom of a stomach ulcer is a burning pain in the center of your chest, typically just below your breastbone. Bloating is also a common symptom, while nausea and vomiting are less frequent symptoms. To diagnose a stomach ulcer, your doctor will ask about your symptoms, take a family history, and do a physical examination. You may also need to undergo an endoscopy, during which a small camera is inserted down your throat while you’re sedated.
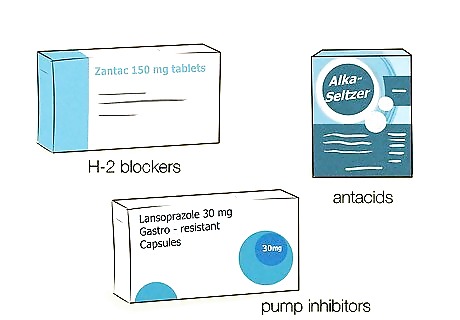
Take one or more acid-reducing medications as recommended. Excess stomach acid doesn’t cause stomach ulcers, but it does make the painful symptoms worse. Cutting back on your stomach acid should reduce your pain and help promote healing of the ulcer. Common acid-reducing options include: Antacids, which are over-the-counter (OTC) medicines that neutralize the acid in your stomach. These don’t really promote healing of your ulcer, but they can help reduce your ulcer pain. H-2 blockers, which reduce the amount of acid secreted into your stomach. These may be prescribed to help reduce discomfort and promote ulcer healing. Proton pump inhibitors (PPIs), which are typically even more effective than H-2 blockers at inhibiting acid secretion. You may be prescribed a PPI for a few weeks or longer to help heal your ulcer.

Take a prescribed antibiotic if you have a bacterial infection. If (and only if) your stomach ulcer is caused by an H. pylori bacterial infection, antibiotics can help reduce your symptoms and heal the ulcer. If your ulcer has another cause, antibiotics will not help. Take any antibiotics exactly as prescribed and for as long as directed. Your doctor may do a breath test to check for signs of an H. pylori infection as part of their diagnosis of your stomach ulcer. In some cases, you may be placed on 2 different antibiotics and a PPI for 2 weeks to treat a stomach ulcer.

Cut back on NSAID pain relievers if they’re causing your ulcer. Stomach ulcers are most commonly caused either by H. pylori infections or frequent use of non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin and ibuprofen. Therefore, reducing or eliminating NSAID use may promote healing of your ulcer. Your doctor will likely advise you to use a different category of pain reliever, such as acetaminophen, instead. If you’re on a doctor-prescribed NSAID regimen, don’t stop taking your medication in an effort to self-treat a suspected ulcer. Always talk to your doctor first.

Drink chamomile tea before you go to bed to help with your pain. Fill a mug with boiling water and use it to steep a bag of chamomile tea for about 4–5 minutes. Drink your tea while it’s still hot to soothe any discomfort you’re feeling from the ulcer. If you want, you can have multiple cups of chamomile tea throughout the day. You can buy chamomile tea from your local grocery store. Chamomile has natural antioxidants and anti-inflammatories so they can reduce your stomach acid and help the ulcer heal faster.
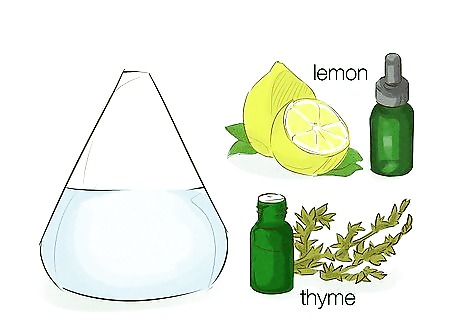
Try aromatherapy with essential oils to ease discomfort. Fill a diffuser with distilled water and a few drops of clove, cinnamon, thyme, or lemon essential oils. As you run the diffuser, take deep breaths so you’re able to relax more and smell the oils. You can use aromatherapy throughout the day or even while you’re asleep.
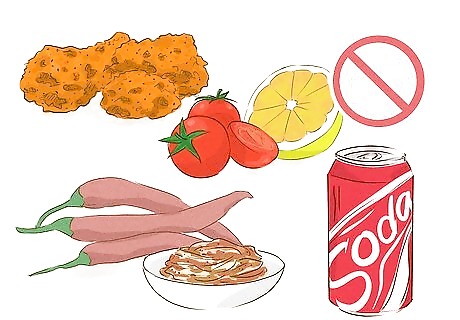
Identify and avoid foods that cause painful flare-ups. Despite what you may have heard, spicy foods don’t cause stomach ulcers—but they can definitely make them feel worse! Different people have different trigger foods that exacerbate their ulcer pain, so your best option is to keep track of what you eat and the severity of your ulcer symptoms. Once you identify particular foods that cause flare-ups, do your best to limit or completely avoid them. Spicy foods, acidic foods (like tomatoes and citrus), chocolate, mint, and fried foods are the most common culprits, but your triggers may be different. Carbonated drinks and dairy products can sometimes soothe ulcer pain temporarily but make it feel even worse afterward. Try keeping a food diary to track what you eat and how you feel afterward. Try an elimination diet where you cut specific foods out of your diet for a few days at a time. If you start feeling more relieved, then try to avoid that food in the future.

Quit smoking and reduce your alcohol intake. In addition to causing a wide range of other health problems, smoking can increase your stomach acid production and worsen your ulcer symptoms. Alcohol also tends to cause extra stomach acid production and therefore more ulcer pain. Steering clear of both may noticeably reduce your symptoms.
Reduce your stress to possibly reduce your ulcer symptoms. Like spicy foods, stress often gets undeserved blame for causing stomach ulcers. While stress isn’t actually the cause, it can definitely make your ulcer discomfort more noticeable. Stress can also trigger unhealthy coping behaviors, like smoking, drinking too much, or eating unhealthy “comfort” foods, that can increase ulcer pain. Look for healthy ways to relieve stress such as light exercise, meditation or prayer, yoga or tai chi, deep breathing, mindfulness techniques, experiencing nature, or talking to a good friend. Talk to your doctor or a mental health professional if you’re really struggling to deal with stress.
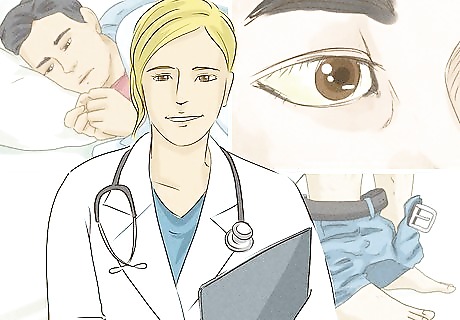
Get additional medical help for ongoing or severe cases. Following a doctor-approved treatment plan may resolve a stomach ulcer in as few as 2-3 weeks, though it may take longer. Stay in contact with your doctor and update them about your progress or lack of progress, and discuss adjustments to your treatment plan as needed. Get medical attention right away if you: Start vomiting blood or dried blood (which looks like coffee grounds). Have persistent vomiting or diarrhea. Develop a high or persistent fever. See blood or dried blood (which looks black and tarry) in your stool. Have severe pain or bloating. Develop jaundice (yellowing of your skin and eyes).


















Comments
0 comment