
views
Initiating Treatment
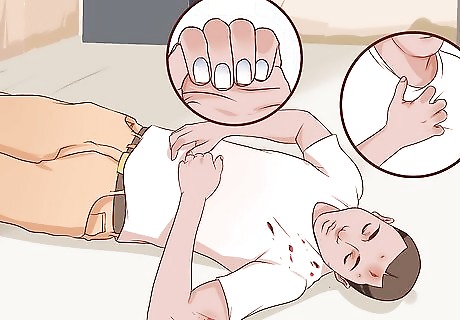
Recognize the symptoms. Before you administer any kind of treatment it's important to know what you're dealing with. Signs and symptoms of shock include the following: Cool, clammy skin that may appear pale or grayish Profuse sweating or moist skin Bluish lips and fingernails Rapid and weak pulse Rapid and shallow breathing Enlarged or contracted pupils (pupils can enlarge in septic shock, but can constrict in traumatic shock) Low blood pressure Low or no urine output If the person is conscious, he or she will display an altered mental status such as being disoriented, confused, anxious, agitated, dizzy, lightheaded, or feel faint, weak, or fatigued The person may complain of chest pain, nausea, and experience vomiting Losing consciousness follows
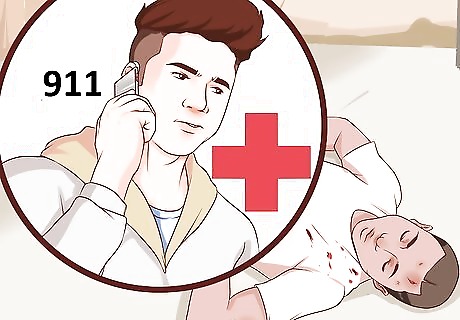
Call 911 or your local emergency services number. Shock is a medical emergency, will require expert medical attention, and hospitalization. You may save the person’s life by ensuring that paramedics are on the way while you initiate treatment. If possible, stay on the line with the emergency services dispatcher to continually provide updates about the person’s condition. Follow the instructions provided by the dispatcher until emergency medical help arrives.

Check for breathing and circulation. Make sure the airway is clear, be sure the person is breathing, and check for a pulse. Observe the person's chest to see if it rises and falls, and place your cheek next to the person’s mouth to check for breath. Continue to monitor the person’s respiration rate at least every 5 minutes, even if they are breathing on their own.
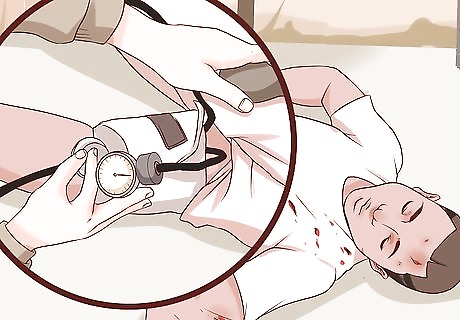
Check blood pressure if possible. If blood pressure equipment should be available and can be used without causing further injury, monitor the person’s blood pressure and report it to the dispatcher.

Start CPR if necessary. Only administer CPR if you are trained to do so. An untrained person may do serious harm to someone by attempting CPR. Only trained people should administer CPR to adults, children, and infants, due to the risk of serious and life-threatening injury. The American Red Cross has recently implemented new protocols for administering CPR. It is important that only people trained in the new methods, and in the use of an AED if available, take charge of administering those procedures.
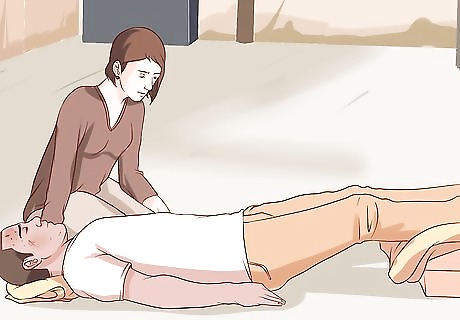
Place the person in the shock position. If the person is conscious and has no injury to the head, leg, neck, or spine, then proceed with placing them in the shock position. Position the person on their back and elevate the legs about 12 inches (30 cm). Do not elevate the head. If raising the legs causes pain, or possible harm, then do not elevate the legs and leave the person lying in a flat position.
Do not move the person. Treat the person where they are unless the surrounding area is dangerous. For safety reasons, you may need to carefully move the person and yourself out of harm’s way. Examples include being located on a highway at the scene of a car accident or near an unstable structure that may collapse or explode. Do not let the person eat or drink anything.
Provide basic first aid to visible injuries. If the person sustained a trauma, you may need to stop the flow of blood from a wound or provide first aid for a broken bone. Apply pressure to any bleeding wounds and dress the wounds using clean materials if available. Wear gloves if you're exposed to blood or other body fluids. This can protect you from potentially harmful bloodborne pathogens.

Keep the person warm. Cover the person with any available material such as towels, jackets, blankets, or first aid blankets.

Make the person as comfortable as possible. Loosen any tight fitting clothing such as belts, buttoned pants at the waist, or any tight clothing around the chest area. Loosen collars, remove neckties, and unbutton or cut away tight clothing. Loosen shoes and remove any tight or constrictive jewelry if on the person's wrists or neck.
Monitoring the Person Until Help Arrives

Stay with the person until help arrives. Do not wait to see if symptoms progress to evaluate the person’s condition, initiate treatment, and monitor their progress or decline.. Talk to the person calmly. If the person is conscious, talking to them can help you to continue to evaluate their condition. Continue to provide updates to the dispatcher on the person’s level of consciousness, their respirations, and pulse.
Continue your treatment. Check and maintain a clear airway, monitor their breathing, and keep check on their circulation by checking the pulse. Monitor their level of consciousness every few minutes until the paramedics arrive.
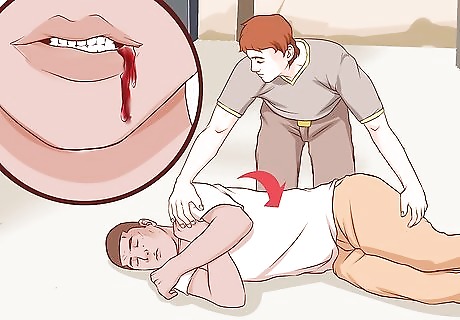
Prevent choking. If the person vomits or is bleeding from the mouth, and there is no suspicion of spinal injury, turn the person onto their side to keep the airway clear and prevent choking. If spinal injury is suspected and the person is vomiting or bleeding from the mouth, clear the airway if possible without moving their head, back, or neck. Place your hands on each side of the person’s face and gently lift their jaw and open the mouth with your fingertips to clear the airway. Be careful not to move their head and neck. If you cannot clear their airway, get help to use a log-rolling maneuver to roll them onto their side to prevent choking. One person should try to keep the head and neck supported and in line with the back as a straight unit, while another person gently rolls the injured person onto their side.
Treating Anaphylaxis
Recognize the symptoms of an allergic reaction. The reaction begins within seconds or minutes after exposure to the allergen. Symptoms of an anaphylactic reaction include the following: Pale skin, possibly flushed or reddened areas, hives, itching, and swelling at the site of exposure. Feeling of warmth. Difficulty swallowing, sensation of having a lump in your throat. Difficulty breathing, coughing, wheezing, and chest tightness or discomfort. Swelling of the tongue and mouth area, nasal congestion, and facial swelling. Dizziness, light headedness, anxiousness, and slurred speech. Abdominal pain, nausea, vomiting, and diarrhea. Palpitations, and a weak and rapid pulse.
Call 911 or your local emergency services number. Anaphylaxis is a medical emergency, will require expert medical attention, and possibly hospitalization. Anaphylaxis can lead to death if it is not treated immediately. Stay on the line with emergency services for further instructions as you administer treatment. Do not delay in seeking emergency medical treatment, even if symptoms appear mild. In some cases, the reaction may be mild at first, then reach a serious and life-threatening level several hours after exposure. The initial reaction involves swelling and itching at the site of exposure. For an insect sting, this will occur on the skin. For a food or drug allergy, the swelling will likely begin in the mouth and throat area, which can quickly interrupt the ability to breathe.
Inject epinephrine. Ask the person if they have an epinephrine autoinjector, such as an EpiPen. The shot is usually administered in the thigh. This is a shot that administers a dose of life-saving epinephrine to slow down the reaction, and is frequently carried by people with known food and bee sting allergies. Do not assume this injection will be enough to completely stop the reaction. Proceed with treatment accordingly, including seeking emergency medical attention.
Talk to the person in a calm and reassuring manner. Try to determine the cause of the reaction. Common allergies that can cause life-threatening anaphylactic reactions include bee or wasp stings, insect bites or stings such as fire ants, food items including peanuts, tree nuts, shellfish, and soy or wheat products. If the person is unable to speak or respond, check for a medical alert necklace, bracelet, or wallet card. If the cause is from an insect or bee sting, scrape the stinger from the skin using something firm, like a fingernail, key, or credit card. Do not remove the stinger with tweezers. This will squeeze more venom into the skin.

Proceed with steps to prevent shock. Position the person flat on the ground or floor. Do not place a pillow under their head since this can interfere with their breathing. Do not give the person anything to eat or drink. Raise their feet about 12 inches (30 cm) off the ground, and cover the person with something warm such as a coat or blanket. Loosen any restrictive clothing such as belts, neck ties, buttoned pants, collars or shirts, shoes, and jewelry around the neck or wrist. If an injury is suspected to the head, neck, back, or spine, do not raise their legs, just let the person remain flat on the ground or floor.
Roll the person on their side if they begin to vomit. To prevent choking and maintain their airway, roll the person on their side if they begin to vomit or if you notice blood in the mouth. Take precaution to prevent further damage if a spine injury is suspected. Get help to gently log-roll the person onto his or her side by keeping the head, neck, and back in as straight a line as possible.

Continue to maintain a clear airway and monitor respirations and circulation. Even if the person is breathing on their own, continue to monitor the rate of respirations and the pulse rate every few minutes. Also monitor the person’s level of consciousness every few minutes until the paramedics arrive.

Start CPR if necessary. Only administer CPR if you are trained to do so. An untrained person may do serious harm to someone by attempting CPR. Only trained people should administer CPR to adults, children, and infants, due to the risk of serious and life-threatening injury. The American Red Cross has recently implemented new protocols for administering CPR. It is important that only people trained in the new methods, and in the use of an AED if available, take charge of administering those procedures.

Stay with the person until the paramedics arrive. Continue to talk to the person in a calm and reassuring manner, monitor their condition, and watch closely for changes. The medical professionals will want an update from you on your observations and steps you have taken to treat this medical emergency.



















Comments
0 comment