views
X
Trustworthy Source
Centers for Disease Control and Prevention
Main public health institute for the US, run by the Dept. of Health and Human Services
Go to source
Examining the differences and similarities between type 1 and type 2 diabetes can help you better understand your condition. Then, you can work with your doctor to create the right treatment plan for you.
Examining the Differences
Expect type 1 to start quickly, while type 2 develops over time. Most people who have type 1 diabetes will experience an acute episode as their body loses the ability to make insulin. This means their symptoms will start suddenly and all at once. However, people with type 2 diabetes usually have symptoms that slowly develop as their condition starts and then worsens. If you think you’re experiencing diabetes symptoms, see your doctor immediately. Keep in mind that type 2 diabetes may not show symptoms at first.
Know type 1 means your body doesn’t produce enough insulin. Type 1 diabetes is an autoimmune condition in which your body’s own immune system attacks the cells in your pancreas that make insulin. After these cells are gone, your body cannot make insulin, which is necessary to manage your blood sugar. This means your body can’t regulate its blood sugar. If you have type 1 diabetes, your body makes either too little or no insulin. Type 1 diabetes is considered an autoimmune disease.
Recognize type 2 diabetes means your body can’t properly use insulin. Your body can become resistant to insulin over time. This means your body must produce more and more insulin to regulate your blood sugar. In some cases, this can overwork your pancreas, causing it to stop making enough insulin. If you have type 2 diabetes, your body is either resistant to the insulin your body makes, meaning it can’t use it properly, or your body no longer makes enough insulin. Type 2 diabetes is a metabolic disease.

Realize type 1 diabetes is more commonly diagnosed in younger people. Type 1 diabetes is usually diagnosed in children, adolescents, and young adults. It can develop in older adults, but typically occurs at a younger age. While type 1 diabetes is usually diagnosed at a young age, it won't go away just because you get older. You'll have type 1 diabetes for the rest of your life. People who are diagnosed with type 1 diabetes are often at a normal or low body weight.
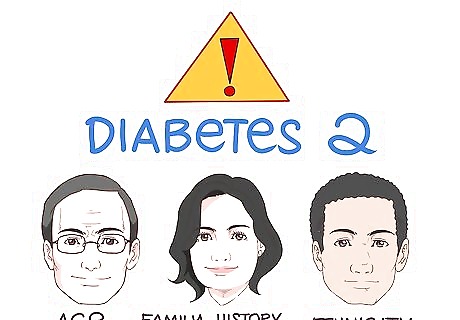
Know type 2 diabetes occurs at any age but usually affects older adults. Type 2 diabetes develops over time as your body becomes resistant to insulin or stops making enough. It can happen to anyone. Although it’s more common in older adults, children, adolescents, and young adults can all develop this condition, as well. You’re more likely to develop type 2 diabetes at a young age if you have risk factors for it. Common risk factors for type 2 diabetes include carrying excess weight, inactivity, age, family history, and being of African, Hispanic, Native American, or Asian descent.
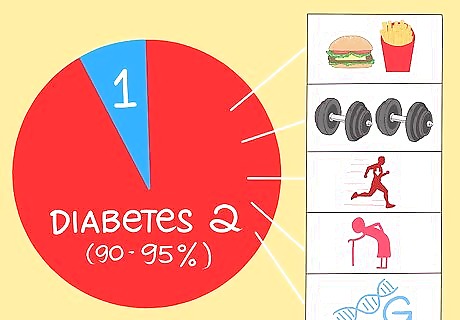
Notice that type 2 diabetes is much more common than type 1. About 90 to 95% of people who have diabetes will have type 2. It usually develops as people age. In most cases, people with type 2 diabetes become insulin resistant due to lifestyle choices, such as eating an unhealthy diet, carrying extra weight, and getting too little exercise. Some people will develop type 2 diabetes due to aging and genetics, despite living a healthy lifestyle.
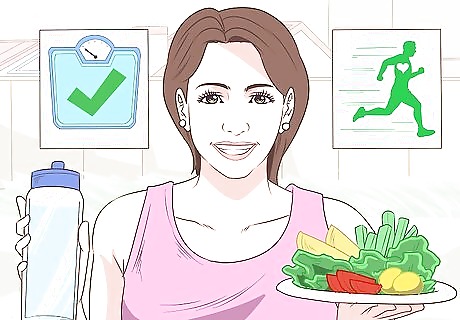
Realize that type 2 diabetes is often preventable, but type 1 isn’t. Lifestyle factors play a bigger role in the development of type 2 diabetes, so you may be able to prevent it. Maintaining a healthy weight, exercising for 30 minutes a day, and eating a healthy diet can help you reduce your risk of developing type 2 diabetes. However, type 1 diabetes cannot be prevented, as it’s caused by an autoimmune reaction in your body that you can’t control. Keep in mind that some risk factors for type 2 diabetes, such as age, family history, and race, are out of your control. You may not be able to prevent type 2 diabetes, so don’t feel bad if you get it. Diabetes is a common condition.
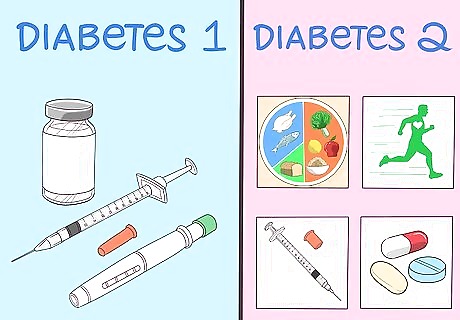
Recognize type 1 always requires insulin, while type 2 may not. If you have type 1 diabetes, your body is not making the insulin it needs, so you’ll need to use insulin therapy. However, people with type 2 diabetes may have options, including diet and exercise, oral medications, and insulin therapy. Your doctor will help you figure out how to best address your diabetes symptoms. Always take your medication as directed by your doctor. Don’t try to change your treatment plan on your own, as this can lead to complications.
Recognizing the Similarities
Realize that both types can be hereditary. Your family history of diabetes plays a role in whether or not you’ll develop the condition. Though genetics are linked to both types of diabetes, type 2 diabetes is less tied to family history than type 1 diabetes. Having a relative with diabetes does not mean you will automatically get the condition. It just means you might be at a higher risk than someone who doesn’t have a family history of the condition.
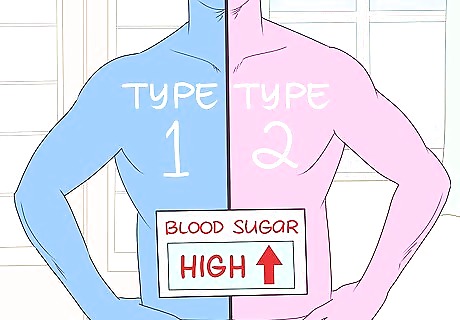
Recognize both types mean your body can’t regulate its blood sugar. When you consume glucose, your body uses insulin to process it. The insulin delivers glucose to the cells in your body to be used as fuel. However, your body can’t process glucose if it doesn’t have enough insulin or if your body loses its sensitivity to insulin. When that happens, diabetes occurs. When you have either type 1 or type 2 diabetes, your blood sugar will consistently be high. Your body isn’t able to keep your blood sugar in a normal range.
Notice that both types can lead to the same complications. You can prevent or delay many diabetes complications with tight glycemic control, such as by taking your medication, monitoring your blood sugar, eating a healthy diet, and exercising for at least 30 minutes a day. However, diabetes can cause serious complications if it's left unchecked. If your diabetes is unmanaged, it can lead to the following conditions: Heart attack Diabetic retinopathy (vision problems and possibly blindness) Dyslipidemia (high cholesterol) Stroke Nerve damage Hypertension (high blood pressure) Heart disease Kidney damage Foot ulcers and skin infections Amputation of limbs, such as toes or feet
Creating a Treatment Plan with Your Doctor

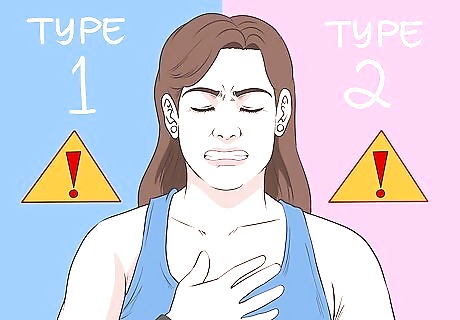
Recognize the symptoms of type 1 diabetes. Usually, type 1 diabetes starts suddenly and causes acute symptoms. It's more likely to occur in younger people, such as children, adolescents, and young adults. Here are the common symptoms of type 1 diabetes: Extreme thirst or hunger Frequent urination Weight loss Extreme weakness Fatigue Nausea Vomiting Irritability Blurred vision Frequent infections, such as fungal skin infections

Watch for the symptoms of type 2 diabetes. Type 2 diabetes can happen at any age, though it's more common in older adults. It develops over time, so you may notice symptoms emerge slowly and many people do not even have symptoms. Call your doctor if you experience the following symptoms: Extreme thirst or hunger Frequent urination Weight loss Extreme weakness Fatigue Nausea Vomiting Irritability Blurred vision Skin infections Slow healing sores Dry, itchy skin Tingling and numbness in your hands and feet
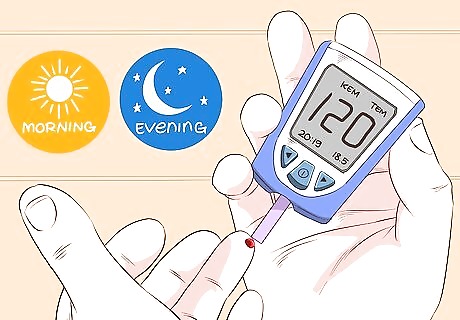
Monitor your blood sugar. Your doctor will tell you when to check your blood sugar. At the minimum, you'll need to check it in the morning and in the evening before bed. In some cases, your doctor may recommend you check it before or after meals. Keep track of your blood sugar so you can watch for patterns. People who are using insulin usually need to check their blood sugar more often than those who aren't.

Talk to your doctor about insulin therapy. Whether you have type 1 or type 2 diabetes, you will likely need insulin therapy. Insulin must be injected for it to be useful, as your body will metabolize it if you take it orally. Your doctor will help you decide if you want to inject yourself with insulin or use an insulin pump. Most people inject insulin with a very thin needle that looks similar to a pen. If you use a pump, you'll wear a cellphone-sized device that pumps insulin into your body through a tube. Insulin therapy may make you uncomfortable, but it won't be painful. If you have type 1 diabetes, you will need insulin therapy to manage your blood sugar. However, you may not need insulin if you have type 2 diabetes. Your doctor will determine which treatment you need.

Take oral medications if prescribed by your doctor. If you have type 2 diabetes, your doctor will likely start your treatment with oral medications. Your doctor can prescribe oral medications that increase your insulin production or make your body more sensitive to insulin. These medicines may also release glucose from your liver while suppressing your insulin production, which means your body is able to transport the glucose with less insulin. Always take your medication as directed. Don't stop taking your medications without approval from your doctor.
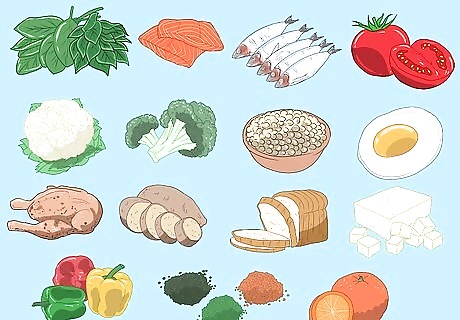
Eat a healthy diet. Eating a balanced diet is important for both types of diabetes. Eat smaller portions at each meal, and spread out your meals throughout the day to keep your blood sugar levels stable. Build your meals around non-starchy vegetables, as well as a lean protein. When you eat carbs, combine them with a protein. The best vegetables for your meals include leafy greens, peppers, root vegetables, tomatoes, and cruciferous vegetables, like broccoli and cauliflower. Choose lean proteins like chicken, turkey, fish, eggs, low-fat dairy, nuts, seeds, beans, legumes, and meat substitutes, like tofu. Include fruit and whole grains in your diet, but measure your servings to make sure you don't consume too many carbs at once.
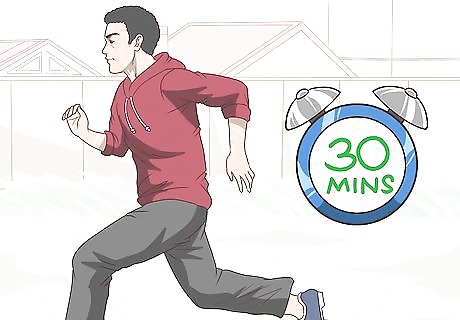
Exercise for at least 30 minutes a day. Exercise is important for managing your condition because it helps you maintain your weight and lowers your blood sugar. Aerobic activity actually transports the sugar in your blood to your muscles and tissues to help power your body. Additionally, it helps your body become more sensitive to insulin. It's okay to break up your exercise into several 10 minute blocks spread throughout the day. For example, you can walk, do aerobics, swim, take a gym class, or dance.

Manage your stress levels to prevent blood sugar spikes. Stress is a normal part of life. However, stress causes your body to release hormones that interfere with how insulin is used. This means stress can spike your blood sugar. You can lower your stress levels by using relaxing techniques like these: Engage in hobbies Play with your pets Sip on a cup of hot tea Color in an adult coloring book Express yourself creatively Read a book Soak in a hot bath Meditate Do yoga Journal Talk to a friend
















Comments
0 comment