views
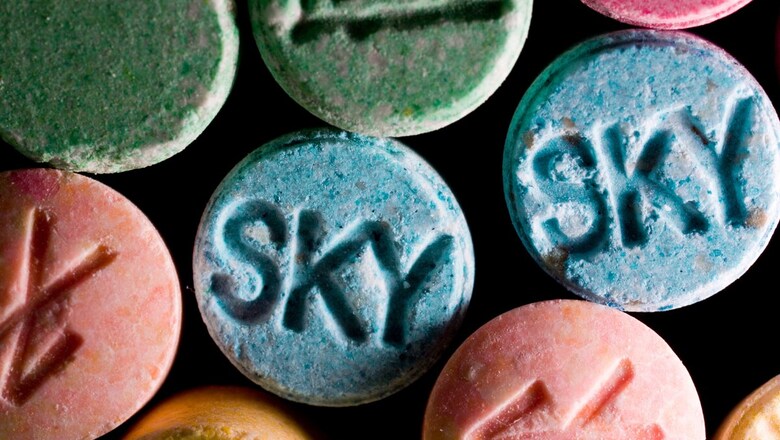
Australia on Saturday became one of the first countries in the world to allow the use of MDMA and magic mushrooms for medical treatment, in a bid to tackle certain mental health conditions.
From July 1, authorised psychiatrists will be able to prescribe the drugs, also known as ecstasy and psilocybin, for the treatment of post-traumatic stress disorder and some types of depression.
Authorities in Canada and the United States allow the medical use of one or both of the drugs, but only in clinical trials or with special permits.
In February, Australia reclassified the drug entirely, after the country’s Therapeutic Goods Administration said trials had found the substances to be “relatively safe” when used in a “medically-controlled environment”.
Supporters of the move hope the drugs can provide breakthroughs for mental health patients, when other treatments have failed.
Mike Musker, a mental health and suicide prevention researcher at the University of South Australia, told AFP that MDMA would be useful for treating post-traumatic stress, while psilocybin can help with depression.
He explained that MDMA “gives people a feeling of connectedness and it makes it easier for people to connect with a therapist and also talk about some bad personal experiences”.
Psilocybin gives patients a “psycho-spiritual effect, which you wouldn’t get on traditional drugs”, he said, adding that this “might make you feel differently about yourself, and your life… and hopefully, it will make you want to live”.
Musker doubts the drugs will be in widespread use among patients until 2024, and said the process would not be a case of “take a pill and go away”.
MDMA, for example, would probably involve three treatments over five to eight weeks, with each session lasting about eight hours.
He said therapists would stay with patients while they are receiving the drugs during sessions that could cost in the region of Aus$1,000 (US$660) each.
– ‘Lack of options’ –
Doctor David Caldicott, an emergency medicine consultant and clinical drug researcher at the Australian National University, told AFP that the changes put Australia “very much ahead of the pack” in exploring the drugs’ medicinal benefits.
But Susan Rossell, a cognitive neuropsychologist at Swinburne University said that, while the treatments “have got potential”, Australia is “moving ahead five years before it should do”.
She told AFP: “When you look at interventions… for any other kind of disease, whether it’s cardiovascular disease or cancer, you cannot get a drug to market as quickly as this has been done.
“There are no drugs on the market that don’t have phase three and phase four clinical trials — and that is what we’re doing here.”
A Health Department spokesperson told AFP that the decision to change the rules “acknowledged that evidence for the use of these substances in treating mental illnesses is not yet well established”.
“However, the benefits for some patients… will outweigh the risks, and there is currently a lack of options for patients with specific treatment-resistant mental illnesses.”
But patients are being warned not to expect a miracle cure.
“I have read about stories where people have had what you call bad trips or actually they’ve re-experienced their trauma, and so we’ve got to take great caution,” Musker said.
“I think there has to be a warning to the consumer that this is a potential side effect before they take part.”
















Comments
0 comment